Cumulative Survival Rate of Implants Placed “Fully Guided” Using CT-Guided Surgery: A 7-Year Retrospective Study
Abstract:
PURPOSE: To evaluate the cumulative survival rates (CSRs) of dental implants placed “fully guided” using computed tomography (CT)–guided surgery, including cone beam CT (CBCT). MATERIALS AND METHODS: Records, mountings, wax-ups, and scanning appliances were made for patients to wear during CT/CBCT scans following established manufacturer-guided surgery protocols. Virtual planning was performed using either the NobelProcera/NobelClinician® or the SimPlant®/Facilitate™ softwares. Manufacturer-produced stereolithographic guides and implant-specific instrumentation were used to place implants fully guided to planned depths and angulations. Included in the study were 177 patients, who had 796 implants placed fully guided, using 212 surgical guides. RESULTS: Among 796 implants placed, there were 24 failures, for a 96.98% CSR. System CSRs were: NobelActive®, 95.87%; Astra OsseoSpeed™, 96.72%; NobelReplace® Select Tapered, 97.02%; and NobelReplace® Select Straight, 100% (P < 0.05). Maxillary CSR was 97.62%; mandibular CSR was 95.88% (P < 0.05). CSR for standard implants (10 mm to 13 mm) was 97.3%; short implants (≤ 9 mm) was 95.1% (P < 0.05), and long implants (> 13 mm) was 95.2%. Implant diameter CSR was not significant (P > 0.05) for any diameter implant. Full-arch immediately loaded CSR (97.18%) was not different compared to full-arch unloaded (97.20%) (P < 0.05). CONCLUSIONS: 1) Fully guided implant CSR was 96.98%, which is comparable to “freehand” placement; 2) CSRs varied between implant systems; 3) fully guided short and long implants had lower CSRs than standard implants; 4) the diameter of fully guided implants did not affect CSR; 5) fully guided implants in the anterior maxilla and posterior mandible had reduced CSRs; 6) extraction/immediate placement using fully guided surgery had reduced CSRs; and 7) immediate loading fully guided implants did not affect CSRs.
While far more dental implants are placed using conventional planning and “freehand” surgery, the use of computed tomography (CT)–guided technology has grown significantly. Studies have demonstrated the precision and accuracy of CT-guided implant surgery.1-7 Its widespread adoption, however, remains to be seen due to a steep learning curve, time involved, and financial considerations. Because of the technology’s complexity, many in the dental surgical community consider its use primarily for difficult fully edentulous patients or patients with distorted anatomy, structural anatomic issues, or questions of bone volume. Additionally, concerns exist regarding cooling irrigation,8 bone overheating,8 an inability to measure insertion torques, keratinized gingival deficiencies,9 and a lack of tactile sense10 when placing implants. These factors might lead one to hypothesize that use of this technology to place implants could negatively impact their cumulative survival rates (CSRs). This report seeks to address this concern.
The CSR of implants placed freehand versus guided implant placement in the pterygomaxillary region has been studied retrospectively.11 Low CSR differences between the two approaches suggest guided surgery is a viable and recommended option. Valente et al showed that slight mean deviations of the planned implant positions in the coronal and apical regions and angulation deviations could be expected.12
The Third European Academy of Osseointegration (EAO) consensus on Computer-Guided Implant Therapy and Soft- and Hard-Tissue Aspects evaluated the accuracy of guided implant placement and stated that: guided surgery does not guarantee precise implant placement; different degrees of deviation should be expected; multiple templates increase inaccuracy compared to one template; and bone-supported templates can provide less accuracy.13
Given the contradictory results reported on CT-guided surgery and the lack of literature on CSRs of implants placed using fully guided instrumentation and surgery, this article compares the differences in CSRs of implants placed “fully guided” with regard to implant system, implant type and dimension, anatomic region, time of insertion, and time of load application.
Materials and Methods
Patients were treated in one private oral and maxillofacial surgery practice from November 2005 through 2012. Patients included fulfilled the following criteria:
Inclusion Criteria
Patients’ implants were placed “fully guided,” which was defined as: use of major implant manufacturer–designed and –produced implant-specific drilling instrumentation, with implant-specific implant mounts, for implant placement through a manufacturer-produced stereolithographic surgical guide, to final depth and angulation. Lack of available instrumentation excluded the following implant systems from inclusion in this study: Endopore® (Sybron Implant Solutions, www.sybronimplants.com), NobelActive™ 3.0 (NobelBiocare, www.nobelbiocare.com), Astra OsseoSpeed™ 3.0 (DENTSPLY Implants, www.dentsplyimplants.us), and Megagen™ (www.imegagen.com).
To limit error from unfamiliar instrumentation, guided implant systems and instrumentation were restricted to those used to place more than 15 implants fully guided. This excluded NobelBiocare Brånemark® and NobelReplace™ CC (NobelBiocare), Ankylos® (DENTSPLY Implants), and 3i Certain® Tapered (Biomet 3i, www.biomet.com) implants.
Exclusion Criteria
To be consistent regarding the patient population of a busy oral and maxillofacial surgery practice, commonly used exclusion criteria such as uncontrolled diabetes, bleeding disorders, osteoporosis, radiation therapy, immunocompromised states, smokers, previous augmentation procedures, prior implant failures, and bruxism were not excluded. Implant survival was defined as: an implant that was still present in the patient’s mouth a minimum of 12 months after its insertion, using functional loading with a provisional or definitive restoration(s) for a minimum of 6 months, and the absence of pain, mobility, or infection.
In patients whose implants were placed with surgical guides in both jaws, or on whom surgical guides were used on two different dates in the same jaw, each jaw or surgery was counted once.
Protocol
Evaluations, treatment plans, and surgeries were performed following established system-specific guided-surgery protocols, without alteration. Records were taken and mountings were performed to create diagnostic wax-ups of the ideal position(s) of the planned restoration(s). Dental laboratory–fabricated acrylic scanning appliances were created.
When the NobelGuide™ (Nobel Biocare) protocol was used, the double scan technique with a radiographic guide and index with gutta percha fiducial markers was used. In SimPlant®-fabricated Nobel-compatible guides and Astra Facilitate™ (DENTSPLY Implants) guides, barium-impregnated teeth were used using a single-scan technique. Patients wore these appliances during a CT or CBCT scan. When a medical CT scan was used for planning, various machines—all 16-slice or greater—were used. When a CBCT was used, all scans were taken on an iCat™ Next Generation scanner (Imaging Sciences International, LLC, www.i-cat.com), at an 8.9-second scan time, and 0.3 to 0.4 voxels. Virtual treatment planning was performed using the NobelProcera/NobelClinician® (Nobel Biocare) or the SimPlant®/Facilitate™ (DENTSPLY Implants) softwares, based on the surgeon’s choice.
Surgeries were performed under intravenous sedation and/or local anesthesia. Laboratory-fabricated bite registrations for surgical guide positioning and stabilization pins or screws were used. Only NobelBiocare– or Astra Facilitate–manufactured, implant-specific, guided surgery instrumentation was used to place their respective implants. Manufacturer-recommended implant-specific drilling protocols were followed. Implants were placed through the surgical guides to final depth and angulation, attached to appropriate implant mounts.
Patient recalls were weekly or monthly for the first 4 months, then every 3 months for the first 2 years.
Implant Systems and Types / Guide Types
NobelReplace Select Tapered, NobelReplace Select Straight, NobelActive, and Astra OsseoSpeed implants fulfilled the inclusion criteria for implant systems. As there is no consensus in the literature as to what defines a short or long implant, or a narrow, regular, or wide-diameter implant, for the purposes of this study three implant lengths were used: short (≤ 9 mm), standard (10 mm to 13 mm), and long (> 13 mm). An implant diameter of 3.5 mm was considered narrow; 4 mm, 4.3 mm, and 4.5 mm were considered standard; and 5 mm was considered wide.
The guide types used included NobelGuides and SurgiGuides/Facilitate Guides.
Anatomic Distribution
Implants were placed in the maxilla and mandible—anterior (central and lateral incisors and canines) or posterior (premolars and molars.) The US tooth numbering system (Nos. 1 through 32) was used for implant locations. Neither zygomatic nor pterygoid implants were included.
Insertion Times / Load Application Times
Implants inserted in bone that was healed for more than 3 months and implants placed immediately after tooth extraction(s) were included. Immediately loaded (implants loaded the day of insertion) and conventionally loaded implants (implants loaded more than 3 months after healing) were included.
Statistical Analysis
CSR values were calculated using actuarial life table analysis (Altman 1999). Descriptive statistics, including mean values and standard deviations, were used for data presentation. CSRs were determined by the Kaplan-Meier method. The Log-Rank (Mantel-Cox) test was used for curve comparison. Values were considered statistically significant when P < 0.05.
Results
Included in the study were a total of 177 consecutive patients ranging in age between 18 and 85; 68 were men and 109 were women. All had fully guided implant placement, using 212 NobelGuide or SurgiGuide/Facilitate Guides.
Fulfilling the inclusion criteria were 796 implants—505 placed in the maxilla and 291 in the mandible; 503 were NobelReplace Select Tapered, 121 were NobelActive, 50 were NobelReplace Select Straight, and 122 were Astra OsseoSpeed.
A combined CSR of 96.98% (24/796 failures) was obtained.
Implant System / Type
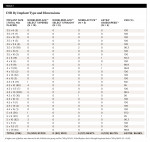
CSRs by implant system were: 97.02% (15/503 failures) for NobelReplace Select Tapered; 100% (0/50 failures) for NobelReplace Select Straight (P < 0.05); 95.87% (5/121 failures) for NobelActive; and 96.72% (4/122 failures) for Astra OsseoSpeed™ (Table 1).
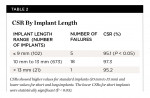
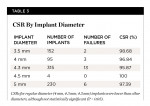
CSRs for short implants (≤ 9 mm) were 95.1% (5/102 failures) (P < 0.05) compared to 97.3% for standard implants (10 mm to 13 mm) (18/673 failures), while CSRs for long implants (> 13 mm) were 95.2% (1/21 failures) (Table 2). Regarding platform diameter, CSRs for 3.5 mm, 4 mm, 4.3 mm, 4.5 mm, and 5 mm were 98.68% (2/152 failures), 96.84% (3/95 failures), 95.87% (13/315 failures), 100% (0/4 failures), and 97.39% (6/230 failures), respectively, which was not statistically significant (P > 0.05) (Table 3).
Anatomic Distribution
CSRs in the maxilla (11/505 failures) were 97.82%, and in the mandible (13/291 failures) 95.53% (P < 0.05). CSR by arch region was 95.53% (8/179 failures) in the anterior maxilla, 99.1% (3/326 failures) in the posterior maxilla, 100% in the anterior mandible (0/40 failures), and 94.82% (13/251 failures) in the posterior mandible (Table 4).
In evaluating tooth/site numbers, CSRs of 98.6% (2/145 failures) were found in the maxillary molars, 99.4% (1/179 failures) in the maxillary premolars, 95.9% (3/74 failures) in the maxillary canines, and 95.3% (5/107 failures) in the maxillary incisors. In the mandible, CSRs of 95.0% (7/140 failures, 6/7 on the left) were found in the mandibular molars, 94.3% (6/106 failures) in the mandibular premolars, and 100% in the mandibular canines and incisors (Table 5).
Insertion Time
Thirty-nine total sites had extractions with immediate implant placement (29 maxilla, 10 mandible) with two failures (CSR 94.87%), both of which were in the maxilla (2/29 failures, CSR 93.10%). In the mandible, a CSR of 100% was found (0/10 failures) (Table 6).
Loading Time
Among 43 complete-arch–reconstruction patients, 34 received implants in the maxilla and nine in the mandible; among a total of 314 implants placed, there were eight failures (CSR 97.45%) (Table 7).
In maxillary complete-arch patients, 107 implants were placed and immediately loaded with provisional restorations (full-arch restoration and All-on-4/5/6), with three failures (CSR 97.20%), while 142 implants were not immediately loaded (full-arch restorations and overdentures), with four implant failures (CSR 97.18%) (P < 0.05). The combined maxillary arch CSR was 97.19% (7/249 failures).
In mandibular complete-arch patients, the CSR for implants placed and immediately loaded was 100% (0/38 failures); 27 full mandibular arch, non-immediately loaded implants were placed, with one failure (CSR 96.29%). Among a total of 65 implants placed in a non-extraction, non-immediately loaded site, there was one failure (CSR 98.46%).
The combined CSR for all complete-arch, fully guided, immediately loaded implants was 97.93% (3/145 failures), which was not statistically significant (P > 0.05) in comparison to the total implant CSR of 96.98%.
Among five All-on-4/5/6 patients—four maxilla and one mandible—there was one failure among the 22 immediately loaded implants with provisional restorations (CSR 95.45%). No failures occurred in the tilted implants placed.
Guide Type
A total of 125 NobelGuides were used for the placement of 555 implants, with 15 implant failures, for a CSR of 97.30%; 87 SurgiGuide/Facilitate Guides were used for the placement of 241 implants, with nine implant failures, for a CSR of 96.27%.
Discussion
The literature is replete with articles discussing the CSRs of implants placed freehand. CSRs have been reported in the 93% ± 5.3% range, with variable follow-up periods, since endosseus root form implants were introduced.14-20 Reports for NobelReplace Select Tapered implants placed freehand and immediately loaded have shown CSRs of 100% after 1 year,21 96.6% after 3 years,22 and 100% after 5 years.23 Although the present study included patients with high risk factors, it still obtained CSR values of 97.02%.
CSRs in the freehand placement of NobelReplace Straight implants were researched in a prospective study comparing healed and post-extraction sites; 210 implants were placed in 59 patients. Among them, 98.05% and 96.52% CSRs, respectively, were found after 10 years.20 In the present study, the CSR for NobelReplace Select Straight implants was 100%, although it included a relatively lower number of fully guided implants inserted.
A CSR of 95.7% has been reported for freehand placement of NobelActive implants in a 3-year study.22 In this study, the data showed a CSR of 95.9% for fully guided placement of NobelActive implants, similar to the results of the previously noted study. The lower CSR for NobelActive implants, in comparison to the other types of implants used in this study, can be explained by the tendency to use this implant in more difficult anatomic problem patients and extraction and immediate placement patients because of its osteotome-like insertion and high initial stability. The steep learning curves for clinicians using this implant system and the differences and nuances in the guided surgery instrumentation are other factors that may have negatively influenced the CSR.
Regarding CSR by implant type, the Kaplan-Meier curve (Figure 1) showed that only the fully guided placement of NobelReplace Select Straight implants had a 100% CSR, with a limited number of implants placed. The other three implant groups had a reduction in CSRs at two time points—between 1 to 4 months and 9 to 12 months. Patient selection, planning, or surgical factors could explain the first decrease; the second decrease could be explained by patient-related factors (ie, medical comorbidities) or prosthetic/restorative considerations.
Implant length affected CSR values. Standard implants placed fully guided had higher CSRs (97.3%) than short implants (95.1%) (P < 0.05) and long implants (95.2%). Despite the large number of standard implants placed (673), short and long implants had almost a two times higher implant loss (6/123 combined failures) in comparison to standard implants (18/673 failures) (P < 0.05).
These results are similar to the data obtained for the freehand placement of short implants using different systems. Straumann short implants (6-mm length) had a 94% CSR after a 72-month follow-up24; AstraTech short implants (6 mm) had a 96.7% CSR after a 12-month follow-up25; and Endopore short implants (7 mm) had an 85.1% CSR after a 60-month follow-up.26
Regarding implant diameter, this study showed lower CSR values (96.13%) (16/414 combined failures) for regular implants (4 mm, 4.3 mm, 4.5 mm), compared to wide (5 mm) (97.39%) or narrow (3.5 mm) (98.68%) implants. This was not statistically significant ( P > 0.05).
These results are similar to a prospective study reporting that the diameter and length of short implants did not affect implant survival after follow-up of 12 to 72 months.27
Implants placed in different tooth positions resulted in different numbers of failures. The right maxillary lateral incisor, left maxillary canine, left mandibular second premolar, and left mandibular first and second molars had more implant failures. These differences are more likely to have been operator related than patient related.
CSR by region of the arch was 95.53% (8/171 failures) in the anterior maxilla, 99.1% (3/326 failures) in the posterior maxilla, 100% in the anterior mandible (0/40 failures), and 94.8% (13/250 failures) in the posterior mandible. A CSR of 98.6% (2/145 failures) was found in the maxillary molars, 99.4% (1/179 failures) in the maxillary premolars, 95.9% (3/74 failures) in the maxillary canines, and 95.3% (5/107 failures) in the maxillary incisors. In the mandible, a CSR of 95% (7/140 failures, 6/7 failures on the left side) was found in the mandibular molars, 94.3% (6/106 failures) in the mandibular premolars, and 100% in the mandibular canines and incisors. These negative differences are likely the result of placing more fully guided implants in narrow soft anterior maxillary bone and in limited bone volume with anatomic nerve proximity problems in the posterior mandible.
A lower CSR was observed in the mandible (95.53%) (13/291 failures) compared to the maxilla (97.82%) (11/505 failures). One explanation could be a better response of the softer, more cancellous maxillary bone to increased temperatures that could occur with fully guided implant insertion, as compared to the dense bone typical of the mandible. Similar results were reported by Slot et al in 2012,28 who found improved CSRs in the freehand placement of posterior maxillary implants supporting overdentures (CSR 99.3%) compared to anterior maxillary implants supporting overdentures (CSR 98%).
An overall CSR of 94.87% was obtained when evaluating implants placed immediately into extraction sockets. Maxillary implants (CSR 93.10%) were more affected than mandibular implants (CSR 100%). In comparison with the total implant 96.98% CSR, immediate implant insertion resulted in a reduction in CSR of 2.11%.
Fully guided, immediately loaded implants showed lower CSR values in the maxilla (97.20%) (3/107 failures) than in the mandible (100%) (0/38 failures). The combined CSR for all fully guided, immediately loaded implants was 97.93% (3/145 failures.) This difference was not statistically significant (P > 0.05) in comparison to the total implant CSR of 96.98%.
Similar results were reported by Vervaeke et al in 2013,29 who found that immediate loading resulted in higher CSRs (98%) with limited peri-implant bone loss after 2 years.
Failures
When examining the 24 reported implant failures, the following observations were made. One implant failed (10/1 failure) in a 65-year-old patient treated with a resection and radiation therapy of 6500 Rads to the maxilla and mandible for a squamous cell carcinoma of the tongue. This patient was treated with hyperbaric oxygen therapy 9 months prior to and again immediately after implant insertion. One failure (4/1 failure) occurred in a 19-year-old patient treated with a block resection and immediate iliac crest block reconstruction for an ameloblastoma of the mandible 6 months prior to implant insertion. One implant failed (5/1 failure) in a 45-year-old female patient who had a failed blade implant, which created a significant mandibular defect, requiring a large allogeneic bone graft to the area 6 months prior to implant insertion. One failure occurred in the authors’ first patient, who was treated with the fully guided surgery instrumentation in 2005 (5/1 failure). Regarding “cluster failures,” six occurred in two patients (10/2 failures, and 9/4 failures) who were 2+ pack-per-day smokers, treated with full-arch maxillary reconstructions. These two patients were the only ones who had more than one implant failure. Had these six patients been excluded from the data, the results of this study would be 171 patients, 762 implants placed, and 14 implant failures, with a total CSR of 98.16%.
Of the 24 implant failures, 12 occurred in eight full-arch patients (six in the two “cluster” patients discussed in the paragraph above), 10 occurred in 10 partially edentulous multiple-unit-patients, and two occurred in two single-unit-restoration patients. Nineteen of 24 implant failures were successfully replaced 4 to 6 months after initial failure. Two implants in fully edentulous patients and two implants in partially edentulous patients were not replaced after failure. In these patients, the decision was made to proceed with the restoration without replacement. One patient, with severe atrophy in the posterior mandible experienced failure of a 4-mm x 6-mm implant. This implant was not replaced and no restoration was attempted. This is the only patient in this series who did not have a restorative success (1/212 restoration failures).
Safety and Accuracy
CT-guided surgery increases safety in implant placement compared to freehand techniques30,31 while being compatible with all aspects of implant surgery, including flapless techniques.32 In 2013, Arisan et al compared errors in implant positioning freehand to computer-aided placement. They concluded that CT-guided surgery may minimize and alleviate errors in freehand implant placement.33 No CT-guided drill-guide technology offers absolute precision. All articles written on stereolithographic guides show deviations between virtual planning and actually obtained implant positions in all dimensions.33 Bone-supported guides have the highest mean deviations, while lower deviations are measured when using mucosa-supported guides.33 The lowest deviations are measured for tooth-supported guides.34 Rigid screw or pin fixation of a single guide, incorporating metal sleeves and implant-specific drilling instrumentation, further minimize deviations.
NobelBiocare first introduced instrumentation for fully guided implant placement in 2005 with the introduction of the NobelGuide technology, workflow, and instrumentation. Since then, most major implant manufacturers have created and marketed instrumentation for the fully guided placement of their implants. Maximizing patient comfort by minimizing traumatic injury to the tissues is the goal of minimally invasive surgery. Flapless insertion of implants has been reported to minimize complications arising from soft-tissue elevation such as infection, dehiscence, and soft- and hard-tissue necrosis.33-35 Additionally, using a flapless technique with surgical guidance, as compared to a non-guided flapless technique, has been reported to minimize the potential injury to underlying anatomy during the implant site osteotomy and implant placement.36
Potential errors, which are additive, can be found in each step in the CT-guided surgery workflow.3,6 Consistent success with CT-guided surgery requires understanding the rationale for all steps in the workflow, attention to detail, meticulously following established recommended protocols, and avoiding skipping steps.37
Conclusions
Within the limitations of this study it is possible to conclude the following: 1) CSR for fully guided implants was 96.98%, which is comparable to data reported for freehand implant placement; 2) CSR for fully guided implant placement was affected by the implant system utilized; 3) fully guided short and long implants resulted in lower CSRs than standard-length implants; 4) the diameter of fully guided implants did not affect CSR; 5) fully guided implants placed in the anterior maxillary and posterior mandibular regions resulted in lower CSRs; 6) extraction with immediate implant placement using fully guided surgery resulted in a reduced CSR; and 7) immediate loading of implants placed fully guided did not affect CSRs.
DISCLOSURE
The authors report no source of study funding from individuals, manufacturers, institutions, or institutional departments. Drs. Orentlicher and Abboud have received speaker's honoraria from NobelBiocare and DENTSPLY Implants, respectively.
ABOUT THE AUTHORS
Gary Orentlicher, DMD
Section Chief, Division of Oral and Maxillofacial Surgery, White Plains Hospital, White Plains, New York; Private Practice, New York Oral, Maxillofacial, and Implant Surgery, Scarsdale, New York
Andrew Horowitz, MD, DMD
Associate Attending, White Plains Hospital, White Plains, New York; Private Practice, New York Oral, Maxillofacial, and Implant Surgery, Scarsdale, New York
Douglas Goldsmith, DDS
Section Chief Emeritus, Division of Oral and Maxillofacial Surgery, White Plains Hospital, White Plains, New York; Private Practice, New York Oral, Maxillofacial, and Implant Surgery, Scarsdale, New York
Rafael Delgado-Ruiz, DDS, MSC, PhD
Assistant Professor, Department of Prosthodontics and Digital Technologies, School Of Dental Medicine, Stony Brook University, Stony Brook, New York
Marcus Abboud, DMD, PhD
Associate Professor and Chair, Department of Prosthodontics and Digital Technologies, School Of Dental Medicine, Stony Brook University, Stony Brook, New York
REFERENCES
1. van Steenberghe D, Glauser R, Blombäck U, et al. A computed tomographic scan-derived customized surgical template and fixed prosthesis for flapless surgery and immediate loading of implants in fully edentulous maxillae: a prospective multicenter study. Clin Implant Dent Relat Res. 2005;7 suppl 1:S111-S120.
2. Rosenfeld AL, Mandelaris GA, Tardieu PB. Prosthetically directed implant placement using computer software to ensure precise placement and predictable prosthetic outcomes. Part 3: Stereolithographic drilling guides that do not require bone exposure and the immediate delivery of teeth. Int J Periodontics Restorative Dent. 2006;26(5):493-499.
3. Abboud M, Wahl G, Guirado JL, Orentlicher G. Application and success of two stereolithographic surgical guide systems for implant placement with immediate loading. Int J Oral Maxillofac Implants. 2012;27(3):634-643.
4. Sarment DP, Sukovic P, Clinthorne N. Accuracy of implant placement with a stereolithographic surgical guide. Int J Oral Maxillofac Implants. 2003;18(4):571-577.
5. Fortin T, Bosson JL, Coudert JL, Isidori M. Reliability of preoperative planning of an image-guided system for oral implant placement based on 3-dimensional images: an in vivo study. Int J Oral Maxillofac Implants. 2003;18(6):886-893.
6. Abboud M, Guirado JL, Orentlicher G, Wahl G. Comparison of the accuracy of cone beam computed tomography and medical computed tomography: implications for clinical diagnostics with guided surgery. Int J Oral Maxillofac Implants, 2003;28(2)536-542.
7. Ersoy AE, Turkyilmaz I, Ozan O, McGlumphy E. Reliability of implant placement with stereolithographic surgical guides generated from computed tomography: clinical data from 94 implants. J Periodontol. 2008;79(8):1339-1345.
8. dos Santos P, Queiroz TP, Margonar R, et al. Guided implant surgery: what is the influence of this new technique on bone cell viability? J Oral Maxillofac Surg. 2013;71(3):505-512.
9. Maló P1, Rigolizzo M, Nobre Md, et al. Clinical outcomes in the presence and absence of keratinized mucosa in mandibular guided implant surgeries: a pilot study with a proposal for the modification of the technique. Quintessence Int. 2013;44(2):149-157.
10. Tal H, Schicho K, Shohat M. Implant locating and placement based on a novel tactile imaging and registration concept: a technical note. Int J Oral Maxillofac Implants. 2007;22(6):1007-1011.
11. Balshi T, Wolfinger G, Slauch R, Balshi S. A retrospective comparison of implants in the pterygomaxillary region: implant placement with two-stage, single-stage, and guided surgery protocols. Int J Oral Maxillofac Implants. 2013;28(1):184-189.
12. Valente F, Schiroli G, Sbrenna A. Accuracy of computer-aided oral implant surgery: a clinical and radiographic study. Int J Oral Maxillofac Implants. 2009;24(2):234-242.
13. Sicilia A, Botticelli D, Working Group 3. Computer-guided implant therapy and soft- and hard-tissue aspects. The Third EAO Consensus Conference 2012. Clin Oral Implants Res. 2012;23 suppl 6:157-161.
14. Naert I, Quirynen M, van Steenberghe D, Darius P. A six-year prosthodontic study of 509 consecutively inserted implants for the treatment of partial edentulism. J Prosthet Dent. 1992:67(2):236-245.
15. Boedeker D, Dyer J, Kraut R. Clinical outcome of immediately loaded maxillary implants: a 2-year retrospective study. J Oral Maxillofac Surg. 2011;69(5):1335-1343.
16. Pozzi A, Sannino G, Barlattani A. Minimally invasive treatment of the atrophic posterior maxilla: a proof-of-concept prospective study with a follow-up between 36 and 54 months. J Prosthet Dent. 2012;108(5):286-297.
17. Davarpanah M, Martinez H, Etienne D, et al. A prospective multicenter evaluation of 1,583 3i implants: 1- to 5-year data. Int J Oral Maxillofac Implants. 2002;17(6):820-828.
18. Davarpanah M, Martinez H, Celletti R, et al. Osseotite implant: 3-year prospective multicenter evaluation. Clin Implant Dent Relat Res. 2011;3(2):111-118.
19. Levin L, Sadet P, Grossmann Y. A retrospective evaluation of 1,387 single-tooth implants: a 6-year follow-up. J Periodontol. 2006;77(12):2080-2083.
20. Degidi M, Nardi D, Piattelli A. 10-year follow-up of immediately loaded implants with TiUnite porous anodized surface. Clin Implant Dent Relat Res. 2012;14(6):828-838.
21. Ostman PO, Hellman M, Sennerby L. Direct implant loading in the edentulous maxilla using a bone density-adapted surgical protocol and primary implant stability criteria for inclusion. Clin Implant Dent Relat Res. 2005;7(suppl 1):S60-S69.
22. Arnhart C, Kielbasa AM, Martinez-de Fuentes R, et al. Comparison of variable-thread tapered implant designs to a standard tapered implant design after immediate loading. A 3-year multicentre randomised controlled trial. Eur J Oral Implantol. 2012;5(2):123-136.
23. Mura P. Immediate loading of tapered implants placed in postextraction sockets: retrospective analysis of the 5-year clinical outcome. Clin Implant Dent Relat Res. 2012;14(4):565-574.
24. ten Bruggenkate CM, Asikainen P, Foitzik C, et al. Short (6-mm) nonsubmerged dental implants: results of a multicenter clinical trial of 1 to 7 years. Int J Oral Maxillofac Implants. 1998;13(6):791-798.
25. Guljé F, Raghoebar GM, Ter Meulen JW, et al. Mandibular overdentures supported by 6-mm dental implants: a 1-year prospective cohort study. Clin Implant Dent Relat Res. 2012;14(suppl 1):e59-e66.
26. Perelli M, Abundo R, Corrente G, Saccone C. Short (5 and 7 mm long) porous implant in the posterior atrophic mandible: a 5-year report of a prospective study. Eur J Oral Implantol. 2011;4(4):363-368.
27. Monje A, Fu JH, Chan HL, et al. Do implant length and width matter for short dental implants (<10 mm)? A meta-analysis of prospective studies. J Periodontol. 2013;84(12):1783-1791.
28. Slot W, Raghoebar GM, Vissink A, Meijer HJ. Maxillary overdentures supported by anteriorly or posteriorly placed implants opposed by a natural dentition in the mandible: a 1-year prospective case series study. Clin Implant Dent Relat Res. 2014;16(1):51-61.
29. Vervaeke S, Collaert B, De Bruyn H. Immediate loading of implants in the maxilla: survival and bone loss after at least 2 years in function. Int J Oral Maxillofac Implants. 2013;28(1):216-221.
30. Wagner A, Wanschitz F, Birkfellner W, et al. Computer-aided placement of endosseous oral implants in patients after ablative tumour surgery: assessment of accuracy. Clin Oral Implants Res. 2003;14(3):340-348.
31. Arisan V, Karabuda CZ, Mumcu E, Özdemir T. Implant positioning errors in freehand and computer-aided placement methods: a single-blind clinical comparative study. Int J Oral Maxillofac Implants. 2013;28(1):190-204.
32. D’haese J, Van De Velde T, Komiyama A, el al. Accuracy and complications using computer-designed stereolithographic surgical guides for oral rehabilitation by means of dental implants: a review of the literature. Clin Implant Dent Relat Res. 2012;14(3):321-335.
33. Arisan V, Karabuda ZC, Özdemir T. Accuracy of two stereolithographic guide systems for computer-aided implant placement: a computed tomography-based clinical comparative study. J Periodontol. 2010;81(1):43-51.
34. Ozan O, Turkyilmaz I, Ersoy AE, el al. Clinical accuracy of 3 different types of computed tomography-derived stereolithographic surgical guides in implant placement. J Oral Maxillofac Surg. 2009;67(2):394-401.
35. Arisan V, Karabuda CZ, Özdemir T. Implant surgery using bone- and mucosa-supported stereolithographic guides in totally edentulous jaws: surgical and post-operative outcomes of computer-aided vs. standard techniques. Clin Oral Implants Res. 2010;21(9):980-988.
36. Cannizzaro G, Torchio C, Leone M, Esposito M. Immediate versus early loading of flapless-placed implants supporting maxillary full-arch prostheses: a randomised controlled clinical trial. Eur J Oral Implantol. 2008;1(2):127-139.
37. Orentlicher G, Goldsmith D, Abboud M. Computer-guided planning and placement of dental implants. In: Orentlicher G, ed. Digital Technologies in Oral and Maxillofacial Surgery, Atlas of the Oral and Maxillofacial Surgery Clinics of North America. Philadelphia, PA: Elsevier; 2012:53-79.