Implant Advancements for the General Practitioner
Improvements in imaging, software, biomaterials, and more enhanced outcomes
In the United States, more than 35 million people are fully edentulous, and 178 million people are missing at least one tooth. With the life expectancy of baby boomers projected at 87 years, the need for implant dentistry will continue to grow dramatically.1 Evidence that patients are spending more on elective and cosmetic medical/dental treatment than ever before in history suggests that more dentists should be providing implant dental services and treatment. General dentists, who are the public’s primary oral healthcare providers, are in a perfect position to diagnose, create a treatment plan, recommend, refer, and treat patients who would benefit from implant dentistry.
Implant dentistry has come a long way during the past few decades, and general dental practitioners are becoming more involved. Statistics show that the vast majority of implant procedures completed by general practitioners are abutment placement and implant-supported crown insertion. The average number of general dentists who are surgically placing dental implants increased by 21.3% from 2002 to 2006, with the average general dentist placing more than 32 implants in 2006.2 The percentage of general dentists who are surgically placing implants should continue to increase as technological advancements in implant dentistry improve the predictability and safety of these procedures.
Advancements in Diagnosis
Diagnostics have evolved rapidly in dentistry. Better exposure, speed, and calibration of images have allowed general dentists to use advanced digital radiography technology in implantology. Calibration for measurement lengths enables dentists to accurately estimate bone volume prior to surgery. Quick film checks during surgery allow for intraoperative evaluation and safety verification.3
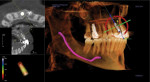
Hounsfield has been credited with the introduction of computed tomography (CT) scanning in 1972. CT technology revolutionized the medical field. With the advent of cone-beam computed tomography (CBCT), both patient exposure to radiation and the machined unit costs were reduced considerably.4 Many general dentists are taking advantage of this technology by using a scanning center, mobile scanning units, or installing it in their dental offices. CBCT technology offers general dentists 3-dimensional (3D) imaging for precise diagnostic and pre-surgical evaluation of the bone volume, density, and anatomic detail (Figure 1).
Implant Software Planning
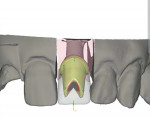
Advances in computer software now allow for precise pre-surgical implant planning.5 Many general practitioners well versed in restorative dentistry are in an excellent position to use CBCT technology to treatment plan implant cases. 3D imaging with scanning appliances facilitates pre-surgical placement planning of dental implants. Implant libraries enable the general dentist to perform virtual implant surgery of practically any implant system (Figure 2).
Many software programs can provide virtual prosthetic wax-ups, eliminating the need to scan appliances for smaller cases. Clinician fabrication of surgical drill guides—whether tooth supported, bone supported, or soft-tissue supported—assist in accurate osteotomy preparation. Although there is now a greater use of CAD/CAM-constructed stereolithographic guides, surgical judgment and training are necessary to evaluate inaccuracies during surgery.6
Biomaterial and Regenerative Advances
Material advances in the biologic regeneratives and implant biomaterials have made dental implant treatment more predictable for clinicians, while advancements in bone grafting materials enable them to maintain and even increase bone volume. With the introduction of particulate mineralized allograft and other grafting materials, socket preservation is now a common predictable clinical procedure.7 General dentists often see patients who require tooth extraction before the specialist and can easily perform or recommend these procedures. Socket grafting maintains bone width and allows for a more predictable implant surgery (Figure 3).
Advances with barrier membranes used in guided bone regeneration (GBR) permit the development of bone volume in both the horizontal and vertical dimension.8 A number of various resorbable and non-resorbable materials are available for GBR (Figure 4). These membranes can be utilized at the time of extraction to maintain horizontal bone width or during augmentation to allow for implant placement.9
Advances in regenerative materials allow for sinus lifting via the crestal or lateral approach.10 Newer instrumentation—such as ostetomes, trephines, diamond drills, reamers drills, crestal approach drilling kits, hydraulic lift devices, peizo electric surgical cutting units, and a plethora of sinus lift instruments—allow simpler and more predictable sinus augmentation. The continuing development of bone regenerative materials allows the placement of implants into sites once considered off-limits for the general dentist.
Advancements by implant manufacturers have made it easier for the general dentist to place and restore implants. Surface enhancements of dental implant design and connections allow the general practitioner to place and restore dental implants more regularly. Smaller-diameter implants—ie, 3.0 mm and smaller—are now available in one- and two-piece designs, allowing general dentists to replace teeth in the narrow bone areas. Shorter-length implants provide general practitioners with new options for the posterior maxilla and mandible.
Advances in Implant Surgery
With the precise surgical planning available today, the placement of implants with the restoration in mind allows a more predictable and esthetic outcome. Small-diameter implants placed with clinical precision using flapless procedures can allow for less morbidity.11 Using minimally invasive incision techniques causes less bleeding and leads to faster postoperative recovery (Figure 5).
One of the most rapidly developing technologies in dentistry is CAD/CAM computer milling. With computer technology, the construction and use of 3D bone models and surgical guides obtained from pre-surgical planning are quickly expanding. As mentioned earlier, these tools are making surgical implant placement more predictable for many general dentists. Surgical guides are a helpful adjunct for the general practitioner for placing implants in proper anatomic and restorative position.
Advances in Prosthetic Abutments And Frameworks
The use of CAD/CAM technology for the construction of prosthetic abutments is increasing. After transferring the position of the implant with direct or indirect implant impression technique, abutments can be fabricated in titanium or zirconium. Computer-milled abutments allow for re-angulations of implant positions for either screw-retained or cementable prostheses.12 Intraoral scanning is increasingly being used by general practitioners for conventional dentistry, and now being used in implant dentistry as well.13
Once the implant position is verified, virtual images allow the general dentist to review the abutment design to determine shape, length, contour, retention, and cement lines prior to fabrication (Figure 6). Modifications to the abutment design can be made before instructing the laboratory to finalize fabrication. Custom abutment implant construction is becoming increasingly affordable and allows for ideal soft-tissue emergence-profile development and improved esthetics (Figure 7).
Overdenture procedures are becoming more popular among general dentists. Narrow-diameter implants have allowed more GPs to place implants with minimally invasive surgery to help retain removable dentures. Overdenture attachment designs are making implant overdenture construction easier. Overdenture bars can now be laser-weld constructed or computer milled. This significantly reduces the cost of conventional cast bar techniques. The computer-milled procedures make removable implant overdenture bar construction simple, accurate, and cost effective.14
CAD/CAM technology for implant prosthetic framework fabrication is becoming more commonly incorporated. Advancements in abutment designs and prosthetic construction have made the implant-supported screw-retained prosthesis much more versatile.15 Newer material choices offer the general practitioner more options. Conventional porcelain-fused-to-metal implant-supported fixed prostheses are still quite popular, although there is a growing interest in titanium and zirconium computer-milled frameworks (Figure 8). These techniques offer the clinician accuracy and durability. The esthetic outcomes of today’s implant-supported prostheses allow general practitioners to become more confidently involved with this evolutionary field.
Conclusion
Dentistry has seen tremendous growth in the use of dental implants for tooth replacement within the profession. Statistics demonstrate an increase in both the restoration and surgical placement of dental implants by general dentists within the United States. Technological advancements in implant dentistry are enabling more general practitioners to be able to predictably and safely provide implant procedures to their patients. Today there are many educational opportunities for the general dentist who wishes to learn more about implant advancements in diagnosis, treatment planning, biomaterials, regenerative biologics, surgery, and prosthetics. As implant advancements continue, the future will see more general practitioners involved in the field.
References
1. Misch CE. Contemporary Implant Dentistry. 3rd ed. St. Louis, MO: Mosby; 2007:8,9;100-110.
2. ADA Survey of Current Issues in Dentistry: Surgical Dental Implant, Amalgam Restoration and Sedation. www.ada.org/~/media/ADA/Science%20and%20Research/HPI/Files/07_scid1.ashx. September 2008. Accessed May 9, 2014.
3. Jeffcoat MK. Digital radiology for implant treatment planning and evaluation. Dentomaxillofac Radiol. 1992;21(4):203-207.
4. Tischler M, Ganz SD. The CT/CBCT-based team approach to care. Part I: Identifying the implant patient and prosthetic options. Dent Today. 2012;31(8):
74,76,78-79.
5. Tucker S, Cevidanes LH, Styner M, et al. Comparison of actual surgical outcomes and 3-dimensional surgical simulations. J Oral Maxillofac Surg. 2010;68
(10):2412-2421.
6. Santana RR, Lozada J, Kleinman A, et al. Accuracy of cone beam computerized tomography and a three-dimensional stereolithographic model in identifying the anterior loop of the mental nerve: a study on cadavers. J Oral Implantol. 2012;38(6):668-676. doi: 10.1563/AAID-JOI-D-11-00130.
7. Minichetti JC, D’Amore JC, Hong AY. Three-year analysis of Tapered Screw-Vent implants placed into extraction sockets grafted with mineralized bone allograft. J Oral Implantol. 2005;31(6):283-293.
8. Rakhmatia YD, Ayukawa Y, Furuhashi A, Koyano K. Current barrier membranes: titanium mesh and other membranes for guided bone regeneration in dental applications. J Prosthodont Res. 2013;57(1):3-14.
9. Elian N, Cho SC, Froum S, et al. A simplified socket classification and repair technique. Pract Proced Aesthet Dent. 2007;19(2):99-104, quiz 106.
10. Li TF. Sinus floor elevation: a revised osteotome technique and its biological concept. Compend Contin Educ Dent. 2005;26(9):619-620, 622, 624-626; quiz 630, 669.
11. Deppe H, Horch HH. Laser applications in oral surgery and implant dentistry. Lasers Med Sci. 2007;22
(4):217-221.
12. Hamilton A, Judge RB, Palamara JE, Evans C. Evaluation of the fit of CAD/CAM abutments. Int J Prosthodont. 2013;26(4):370-380.
13. Syrek A, Reich G, Ranftl D, et al. Clinical evaluation of all-ceramic crowns fabricated from intraoral digital impressions based on the principle of active wavefront sampling. J Dent. 2010;38(7):553-559.
14. Torsello F, di Torresanto VM, Ercoli C, Cordaro L. Evaluation of the marginal precision of one-piece complete arch titanium frameworks fabricated using five different methods for implant-supported restorations. Clin Oral Implants Res. 2008;19(8):
772-779.
15. Cavallaro J Jr, Greenstein G. Angled implant abutments: a practical application of available knowledge. J Am Dent Assoc. 2011;142(2):150-158.
About the Author
John C. Minichetti, DMD
Director, Dental Implant Learning Center
Private Practice
Englewood, New Jersey
Attending, Englewood Hospital
President, American Academy of Implant Dentistry
Diplomate, American Board of Oral Implantology