Proposed Guideline Revisions for Dental Sedation and General Anesthesia:
Why Target the Safest Level of Sedation?
Raymond A. Dionne, DDS, PhD
Recently proposed revisions to the American Dental Association’s Guidelines for the Use of Sedation and General Anesthesia by Dentists, aimed at improving safety in dental offices, differentiate between levels of sedation based on drug-induced changes in physiologic and behavioral states. However, the author of this op-ed is concerned the proposed revisions may have far-reaching and unintended consequences.
Some 45 years ago, public concern regarding the safety of dental sedation and anesthesia prompted the development of guidelines for training1 based on a consensus of expert opinions. Throughout the years, these guidelines have been revised2-4 as new reports of deaths in dental offices arose. Public concern in the 1980s prompted the National Institutes of Health (NIH) to hold a consensus conference, “Anesthesia and Sedation in the Dental Office,”5 resulting in a 1985 statement. In the past decade, worry regarding the safety of enteral sedation was addressed in a jointly sponsored workshop with consensus recommendations for patient safety.6 Despite concerns, the number of hospital-based training general-anesthesia programs available to general dentists has decreased from 227 to approximately10,8 contributing to a gap between the need for general anesthesia for dental patients and the availability of these services.6 This has likely contributed to the increased popularity of enteral sedation, as evidenced by the more than 22,000 dentists trained by the Dental Organization for Continuing Sedation Education since 2000 and other academic-based and proprietary-training programs for conscious sedation,9 which suggest dentists recognize the ongoing need to provide anxiety control in outpatient settings.
Specialists in oral surgery and pediatric dentistry receive sedation education as part of their training and provide varying levels of sedation in their practices, primarily as single-operator anesthetists augmented by minimally trained dental assistants. Although the American Dental Association (ADA) does not include dental anesthesia on its list of recognized dental specialties, dentist-anesthesiologists are well known as being providers of office-based anesthesia services for dentistry and are recognized by the American Board of Dental Specialties. Dentist-anesthesiologists undergo training in a hospital-based, accredited training program that prepares them to deliver the full spectrum of anesthesia to a diversity of patients. Most dentist-anesthesiologists in the United States practice the medical model of anesthesia, in which a dedicated anesthesia provider works with a separate surgeon/operator. The various levels of training, ranging from doctoral training with minimal experience in the use of inhalational and oral sedation, to continuing education for enteral sedation, to training in sedation and anesthesia as part of specialty training, to 2 years of hospital training in anesthesiology, result in a wide array of expertise and experience in the use of sedation and anesthesia in clinical practice.
Recent efforts to improve the safety of sedation in dental offices include ADA Resolution 77, which was rejected by the ADA House of Delegates in 2015 but has been revised for consideration in 2016.10 These proposed revisions of the 2012 ADA Guidelines for the Use of Sedation and General Anesthesia by Dentists differentiate levels of sedation (minimal, moderate, or deep sedation) and general anesthesia based on drug-induced changes in patients’ physiologic and behavioral states. The Educational Requirements (section III) and Clinical Guidelines (section IV) for Minimal Sedation and Moderate Sedation are described separately while the Deep Sedation and General Anesthesia are grouped together, reflecting the similar risks and levels of training required for the level of central nervous system (CNS) and respiratory depression associated with deep sedation and general anesthesia. The type and amount of training for each level of sedation varies widely, from local to general anesthesia. The 4 categories of drug-induced depressed consciousness, along with their associated physiologic consequences, form the basis for designating the number of drugs that can be administered for minimal sedation, the maximum recommended dose (MRD) of a drug administered for minimal sedation, monitoring equipment, and the amount of required training. Minimal sedation is a drug-induced state, and patients can respond normally. Moderate sedation is a drug-induced depression of consciousness, and patients can respond purposefully to verbal commands.
In the absence of reliable estimates of serious morbidity and mortality for sedation and anesthesia performed by dentists, it is not possible to provide assurance to practitioners and the public of the relative safety of the varying levels of depression produced by the wide variety of drugs and doses used by dentists in outpatient settings. Developing recommendations to improve the safety of anesthesia and sedation provided to dental outpatients is hampered by the lack of reliable estimates of serious morbidity and mortality. This problem was first noted more than 30 years ago in the Consensus Statement from the NIH workshop,5 but some argue that the profession has not made enough effort to address the issue. The ability to search online, however, now makes it easier to find reports of death attributable to anesthesia and sedation administered in dental offices. Such publicized deaths are often in healthy patients undergoing elective procedures.11
Individual case reports, reported by the media, identify general anesthesia, parenteral sedation, and multiple-drug combinations as the prevalent causes of death, not orally administered benzodiazepines as the sole agent. While such case reports, in general, provide the lowest level of scientific evidence, these cases make the focus of the guidelines on enteral sedation inconsistent with the intention of improving patient safety by regulating one of the safest drug classes used for sedation—enterally administered benzodiazepines—while ignoring the use of drugs that produce respiratory depression, such as opioids, barbiturates, and general anesthetic agents.
A traditional strategy for reducing adverse drug events is to administer the right drug, to the right patient, at the right dose, via the right route of administration at the right time.12 Arguably, by focusing on the use of enteral sedation by benzodiazepines, the proposed revisions unintentionally may be permissive to the opposite strategy: giving the wrong drugs (not as safe as benzodiazepines), at the wrong dose (not approved for outpatient sedation), and via the wrong route (parenteral administration has a steeper dose response curve and more narrow margin of safety than oral administration).
The proposed difference between training in minimal sedation (16 hours didactic with clinically oriented experiences) and moderate sedation (60 hours didactic and 20 live-patient experiences) is substantial and may inadvertently limit the number of dentists who will be trained in moderate sedation. Increasing training requirements to provide sedation services may perpetuate a fear of dentistry in patients as a barrier to access to care for the substantial portion of patients (~15%) who self-report as “terrified” or “very nervous” about receiving dental care.13
Noteworthy by its omission in these guidelines to improve safety is consideration of scientific evidence for the safety of the drugs and combinations used for moderate and deep sedation and consideration of the incidence of serious morbidity and mortality for drug regimens used clinically. Both of these levels of sedation are defined in the proposed revisions as producing greater decreased consciousness that is associated with decreased respiration and the ability to maintain an airway.
Enteral sedation is most commonly administered with benzodiazepines. This class of sedative-hypnotics produces minimal depression of respiration in comparison to opioids and general anesthetics administered for moderate or deep sedation that inherently depress respiration. It may be more accurate to define the levels of sedation as minimal, moderate, or deep respiratory depression to better characterize their physiologic effects and potential for serious morbidity and mortality.
This editorial discusses the proposed guidelines revisions to improve safety while maintaining dentists’ ability with appropriate training to safely administer anxiolytic drugs to patients in outpatient settings.
Evaluating the Safety of Outpatient Sedation Procedures
Criteria for evaluating efficacy and safety in clinical trials for procedural sedation have recently been described by the Sedation Consortium on Endpoints and Procedures for Treatment, Education, and Research (SCEPTER), a public–private partnership with the US Food and Drug Administration (FDA).14 The SCEPTER group convened a meeting of clinicians, researchers, and regulators with the objective of developing recommendations for procedural sedation. Four core outcome domains were recommended for consideration in sedation clinical trials: safety, efficacy, patient-centered and/or family-centered outcomes, and efficiency. These core outcomes are consistent with 4 of the 6 aims for healthcare described by the Institute of Medicine.15
The expectation for a sedative procedure is that the method be as safe or safer than standard practice for the clinical procedure. Drug-related adverse events associated with the sedative procedure are an important consideration, but the occurrence of serious morbidity or mortality substantially offsets any benefit gained by a sedation procedure, especially for elective procedures. Adverse events such as respiratory depression, apnea, hypoxemia, and hemodynamic instability can occur during procedural sedation in adults and pediatric populations and should be included in the assessment of the safety of drugs used for procedural sedation.14
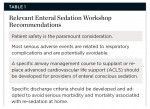
The safety of enteral sedation for dental outpatients was the focus of a workshop6 sponsored by the Anesthesia Research Foundation, the Dental Anesthesiology Research Group of the International Association for Dental Research, and the US Pharmacopoeial Convention, which resulted in recommendations to ensure safety (Table 1). Another widely accepted systematic review from the American Society of Anesthesiologists (ASA) Task Force on Sedation and Analgesia by Non-Anesthesiologists addressed many of the same issues that form the basis for the proposed changes in the guidelines, and in addition specifically addressed the drugs and combinations of drugs used for sedation by non-anesthesiologists.16 Both the large body of evidence reviewed and the consensus of expert opinion indicated that the primary cause of serious morbidity and mortality associated with sedation is due to respiratory depression and airway obstruction. There was also evidence and consensus that the combination of sedative drugs and opioids increase the likelihood of adverse outcomes, including ventilatory depression and hypoxemia. The review suggested that the use of anesthetic induction agents for sedation, such as propofol, methohexital, and ketamine, results in satisfactory moderate and deep sedation, but that avoiding these medications decreases the likelihood of adverse outcomes during moderate sedation.
The ASA Task Force cautions practitioners that methohexital and propofol can produce rapid, profound decreases in level of consciousness and cardiorespiratory function, potentially culminating in a state of general anesthesia. It recommends that even if moderate sedation is intended, patients receiving propofol or methohexital by any route should receive care consistent with that required for deep sedation, and that practitioners should be qualified to rescue patients from any level of sedation, including general anesthesia. The guidelines and precautions from authoritative sources highlight that outpatient sedation drugs that produce respiratory depression and general anesthesia primarily cause the risks. However, the ADA guidelines focus on minimal sedation that is highly unlikely to produce either. They do not address the great risks for respiratory depression and loss of consciousness for doses of opioid drug combinations and anesthetic induction agents used for moderate and deep sedation that exhibit greater potential for serious morbidity and mortality.
The ASA Task Force also stressed that patients may continue to be at significant risk for developing complications after the procedure is complete. Examples of drugs that may result in residual sedation and cardiopulmonary depression include oral and rectal chloral hydrate, a drug commonly used by dentists for pediatric sedation. Continued observation, monitoring, and predetermined discharge criteria decrease the likelihood of adverse outcomes for both moderate and deep sedation after trained personnel release patients from observation.
These published proceedings indicate the importance of avoiding drug-induced toxicity in order to minimize serious morbidity and mortality that results with finite probability when administering drugs for procedural sedation. A large clinical trial comparing single or multiple doses of parenterally administered midazolam to midazolam plus fentanyl or midazolam plus fentanyl and methohexital did not demonstrate any respiratory depression (ie, rate, oxygen saturation, expired carbon dioxide) for midazolam alone but clearly showed respiratory depression when an opioid or a barbiturate were coadministered.17
While the proposed guidelines limit the dose of the safest drug class used for enteral sedation—the benzodiazepines—they do not address doses for opioid drug combinations and anesthetic induction agents that exhibit greater potential for serious morbidity and mortality. Also omitted from the proposed guidelines is the need for discharge criteria for patients who have received moderate or deep sedation with anesthesia induction agents or chloral hydrate. The focus on the safest level of sedation that results in minimal respiratory depression when administered and monitored by an appropriately trained and credentialed dentist to a patient whose risk factors have been prospectively evaluated and the dose adjusted accordingly is not analogous to unmonitored use of a fixed dose at home, which is the basis for the MRD for using triazolam for insomnia. It would be more beneficial to patients to place emphasis on the safety of drugs, doses, and depressed consciousness for moderate and deep sedation rather than ignore the continued use of sedation procedures with greater potential for serious morbidity and mortality.
Maximum Recommended Dose for Outpatient Sedation
An underlying assumption in using the MRD to predict safety and the requisite levels of training is that the recommended dose is for outpatient sedation and based on scientific evidence and regulatory review by the FDA. However, most drugs that are used for sedation of dental outpatients are used off label and have not been evaluated by the FDA for safety and effectiveness for that indication. The FDA is a regulatory agency within the federal government that is responsible for protecting the public health by assuring the safety, efficacy, and security of human and veterinary drugs, biologic products, medical devices, and the nation’s food supply, cosmetics, and products that emit radiation.18 As part of this process, the FDA approves the content of the package insert (also called the “label”) as the official prescribing information. This label describes the approved indications for use of the drug and clinical pharmacology information, including dosage, adverse reactions, and special warnings and precautions. A licensed clinician is not bound by the package insert and may legally prescribe a drug for any purpose he or she deems appropriate.
Demonstrating a drug’s efficacy for a specific indication to the FDA requires performing well-controlled clinical investigations. Determining safety is more complex, as no drug is totally safe; all drugs produce adverse effects in some patients at therapeutic doses. Many serious adverse effects are infrequent and may go undetected in the relatively small samples used in clinical trials for drug approval, which include usually no more than a few thousand participants. The voluntary reporting systems in the United States are not as robust as legally mandated systems in some other countries,19 and few clinicians file adverse drug reports. Moreover, estimates of the incidence of adverse events to predict safety cannot be quantified in the absence of any reliable estimates of adverse events, the amount of drug administrations that occurred, or dosage amounts. Consequently, determining which drugs and doses for an off-label indication are safe and effective is left to clinicians administering the drugs.
Off-Label Use of Sedative-Hypnotics
The use of an approved drug in another dosage form, for another indication, at higher doses, in a different patient population, or for a use that is not in the original labeling is considered to be an off-label use. The FDA recognizes that the off-label use of drugs by practitioners often is appropriate and can result in therapeutic innovation and become a standard practice in the absence of regulatory approval for that use. For example, tricyclic antidepressants were recognized in the 1970s to be effective for relieving chronic pain at doses lower that those used to treat depression and eventually became widely used for the treatment of pain. Some drugs used for oral sedation in dentistry, such as chloral hydrate, were introduced as sedatives before manufacturers were required to show evidence of efficacy in well-controlled trials and demonstrate safety in extensive animal testing and carefully controlled dose escalation studies in humans. Introducing drugs into clinical practice that satisfied these requirements (eg, benzodiazepines) has resulted in drugs that are better suited for anxiety relief versus having nonspecific CNS depression manifesting as sedation, respiratory depression, and decreased consciousness.
Few drugs currently available in the United States have an approved indication for procedural sedation, making the use of most drugs and doses used by dentists for sedation to be non-validated, off-label use from a regulatory perspective. Using the dose from the label for one indication has no logical basis as an indicator of safety for another indication or in a different context. For example, administration of a drug such as propofol by a dentist for outpatient sedation based on its approval as a general anesthetic for use in the operating room by medical anesthesiologists does not convey any assurance of safety or regulatory review for the off-label use.
Safety of Triazolam Used Off-Label for Enteral Sedation
Concerns about the increased use of triazolam for enteral sedation relate to uncertainty surrounding incremental dosing for titration, possible idiosyncratic reactions to triazolam, and the off-label use of a sedative-hypnotic.20 Publicized reports of problems attributed to triazolam were often due to inappropriate prescribing or patient misuse.21-23 The FDA reviewed the drug three times and pronounced it to be safe and effective.24,25 The oral route of administration is generally considered to be the safest route of administration as absorption is more delayed and results in lower peak drug concentrations than parenteral administration.26 The enteral administration of separately delivered and timed doses of triazolam should result in even more gradual onset and lower peak drug levels as redistribution and elimination will have started as the next dose is administered. The published evidence27-29 summarized in Table 2 (view online at dentalaegis.com/go/cced1005) supports enteral administration of benzodiazepines for anxiety relief in the dental office, as does decades of clinical experience by the dental profession.20
Determining the Relationship Between Dose and Patient Responses
Individuals vary in the magnitude of their anxiety toward dentistry (Figure 1) and their responses to the same dose of a drug or to a similar drug from the same class, and even the same individual may respond differently to the same drug dose at a subsequent administration. This is especially true of orally administered drugs. Many factors, including genetics, age, disease, body weight, and the presence of coadministered drugs, influence the variability in the pharmacodynamic response of the population. This variability forms the basis for dose-response curves that illustrate the gamut of responses from a fixed dose that usually are varied. The response to drugs administered for subjective symptoms such as dental pain and apprehension is highly variable and can range from not achieving a therapeutic effect at a fixed dose to developing significant morbidity or even mortality. For example, the range of morphine needed to achieve pain relief following general surgery varies 40-fold when patient-controlled analgesia is used. Dosing recommendations based on mathematical extrapolation to body weight of the patient using maximal dosing recommendations in the FDA-approved package insert or conceptual modeling of pharmacokinetic data are not based on clinical trials that directly measure the dose-anxiolytic response in humans.30,31 While such calculations allow the clinician to better determine the dose based on age and body weight of patients, they do not take into consideration inter-individual variation in pharmacokinetic and pharmacodynamic responses and should be considered as prudent advice from prominent clinicians, not evidence-based recommendations based on scientific literature.
The dose of a drug required to produce a specified effect (such as anxiety relief) in 50% of the population is calculated as the median effective dose. This dose does not predict the response of any given individual in the population but rather serves as a basis for comparing the relative efficacy of the drug to its median toxic dose. The ratio of these calculated median doses is a statement of the therapeutic window and is a reflection of a drug’s selectivity for producing its desired effect versus its adverse effects. For drugs used for sedation, this relationship defines the anxiolytic efficacy of the drug versus its risk of producing compromised ventilation and respiratory depression factors that are often identified as the initiating influences that result in serious morbidity or mortality. Therapeutic success and safety result from integrating efficacy and safety data from animal and clinical studies with individual factors that determine the singular response of a given patient. Extrapolating from a dose determined from population data, such as the MRD, does not directly predict the safety of a drug in an individual patient, especially if based on data for another indication.
A recent example of the hazards of extrapolating across indications and patient populations involved the apparent safety of selective cyclooxygenase-2 (COX-2) inhibitors for short-term use for acute pain and their chronic administration to prevent the development of colon polyps. The unexpected findings of increased cardiovascular events and stroke when administered chronically resulted in their removal from the market and a “black box” warning for virtually all COX-2 inhibitors and non-steroidal anti-inflammatory drugs (NSAIDs).
Guidelines to Improve Sedation Safety: Evidence-Based or Expert Opinion?
While at least one large-scale clinical trial has evaluated the safety of parenteral administration of sedative drugs and combinations,17 only case reports, case series,32 and a retrospective closed-claims study from one dental specialty33 provide very limited evidence for the safety of sedation and anesthesia by dental professions. Conversely, the large number of case reports that exist online, in the files of state dental boards, and in the closed claims of liability insurance carriers provides an accessible database that could readily identify trends in drug-related morbidity and mortality. The author calls on the dental profession to create a verified database of morbidity and mortality of all cases related to sedation and anesthesia in the dental office so that risk factors can be identified and recommendations can be made.
A comparison of office-based anesthesia provided by dentist anesthesiologists to operating-room anesthesia using national outcomes registries provides objective evidence of safety,34 which should be considered when evaluating the safety of the various levels of outpatient sedation performed in the dental office.
Given the widespread recognition for basing dental practices on scientific evidence, the consideration of a return to “eminence-based” clinical practices seems questionable.
The author postulates that the arbitrary use of the MRD for drugs approved for a different therapeutic indication, ie, the induction of sleep, may be a fallacious surrogate endpoint for predicting the safety of drugs used off-label for sedation, determining monitoring requirements, and promulgating training requirements. Dental professionals and their patients deserve policies for training and safety that are based on valid endpoints and an unbiased review of the literature. The scientific evidence on which to support the current dental use of anxiolytic, adjunctive agents and anesthetics, which is sorely lacking, would be greatly enhanced by developing national statistics for morbidity and mortality that differentiate safe drugs and practices from problematic ones for all levels of anesthesia and sedation.
If implemented, the proposed revisions of the guidelines will not appreciably improve the safety of enteral sedation but may eventually limit the ability of general dentists to provide sedation services to patients who would otherwise avoid restorative and preventive dental procedures. This could herald the return to limited treatment options for fearful patients: extractions provided by a small group of specialists who have been trained in parenteral sedation. The lack of a scientific basis for the concept of MRD, the educational evidence for determining competency based on the number of hours or cases performed, or recognition of the dichotomy between the patient-centric outcome of anxiety relief and the observer-rated outcome of sedation should be considered. While questions related to the safety of the single operator-anesthetist had been addressed in medical practice in favor of having a credentialed physician or nurse-anesthetist manage the patient, the oral-surgery community relies on the presence of a minimally trained dental assistant to monitor the patient and administer drugs (under the supervision of the dentist also performing the clinical procedure) that produce respiratory depression or loss of consciousness. The ability to develop guidelines for training and determine the safety of clinical practices is significantly hindered by the lack of reliable morbidity and mortality evidence based on current clinical practices. The medical profession in its efforts to improve the safety of anesthesia and sedation has benefited greatly from information in databases that permit calculation of the morbidity and mortality rate associated with general anesthesia performed in hospitals and outpatient clinics.35,36
Conclusion
Discussion of all potential risk factors that affect the safety of dentists providing anesthesia and sedation in outpatient settings is beyond the scope of this article, but it should be recognized that dictating clinical practice based on the concept of MRD and arbitrary assignment of training hours and clinical experiences are only a few of the many factors that determine the overall risk. Recognition of the need to adequately inform patients of the incidence of death associated with various types of anesthesia and sedation, for example, is now being recognized through legislative efforts in California and Florida and in the insurance liability profession.37 The dental profession and the public would be better served by development of an evidence-based comprehensive strategy to optimize the safety of outpatient anesthesia and sedation rather than attempting to restrict the use of enteral sedation through the proposed revisions to the ADA guidelines.
Acknowledgment
The author would like to thank Mark Saxen, DMD, for his suggestions in the creation of this manuscript.
References
1. American Dental Association, Council on Dental Education. Guidelines for Teaching the Comprehensive Control of Pain and Anxiety in Dentistry. Chicago, IL: American Dental Association; 1971.
2. American Dental Association, Council on Dental Education. Guidelines for Pain and Anxiety Control. Chicago, IL: American Dental Association; 1982.
3. American Dental Association. Guidelines for Teaching Pain Control and Sedation to Dentists and Dental Students. Chicago, IL: American Dental Association; 2007.
4. American Dental Association. Guidelines for the Use of Sedation and General Anesthesia by Dentists. Chicago, IL: American Dental Association; 2012.
5. Dionne RA, Laskin DM. Anesthesia and Sedation in the Dental Office. New York, NY: Elsevier Science Ltd.; 1986.
6. Dionne RA, Yagiela JA, Coté CJ, et al. Balancing efficacy and safety in the use of oral sedation in dental outpatients. J Am Dent Assoc. 2006;137(4):502-513.
7. Dionne RA, Campbell RL. Survey of general anesthesia residency training for dentists. Anesth Prog. 1979;26(1):5-8.
8. American Society of Dentist Anesthesiologists. www.asdahq.org. Accessed August 3, 2016.
9. DOCS Education Website. About us. https://www.docseducation.com/about-us. Accessed August 19, 2016.
10. Council on Dental Education and Licensure. American Dental Association. Call for Comment. Proposed guidelines. https://www.ada.org/~/media/ADA/Education%20and%20Careers/Files/CDEL_ ProposedGuidelines_2016June03.pdf?la=en. Accessed August 15, 2016.
11. Egerton B. Deadly dentistry. Dallas Morning News. December 9, 2015. https://interactives.dallasnews.com/2015/deadly-dentistry/. Accessed August 10, 2016.
12. Osterhoudt KC, Penning TM. Drug toxicity and poisoning. In: Brunton L, Chabner B, Knollman B, eds. Goodman and Gilman’s The Pharmacological Basis of Therapeutics. McGraw Hill, New York, NY. 2011;81.
13. Dionne RA, Gordon SM, McCullagh LM, Phero JC. Assessing the need for anesthesia and sedation in the general population. J Am Dent Assoc. 1998;129(2):167-173.
14. Williams MR, Ward DS, Carlson D, et al. Evaluating efficacy in clinical trials of procedural sedation, part I: Sedation Consortium on Endpoints and Procedures for Treatment, Education, and Research (SCEPTER) recommendations. Anesth Analg. Accepted for publication.
15. Institute of Medicine. Crossing the Quality Chasm: A New Health System for the 21st Century. Washington, DC: National Academy Press; 2001.
16. American Society of Anesthesiologists Task Force on Sedation and Analgesia by Non-Anesthesiologists. Practice guidelines for sedation and analgesia by non-anesthesiologists. Anesthesiology. 2002;96(4):1004-1017.
17. Dionne RA, Yagiela JA, Moore PA, et al. Comparing efficacy and safety of four intravenous sedation regimens for dental outpatients. J Am Dent Assoc. 2001;132(6):740-751.
18. Food and Drug Administration website. What Does FDA Regulate? https://www.fda.gov/AboutFDA/Transparency/Basics/ucm194879.htm. Accessed August 10, 2016.
19. Rivera SM, Gilman AG. Drug invention and the pharmaceutical industry. In: Brunton LL, Chabner BA, Knollman BC, eds. Goodman and Gilman’s The Pharmacological Basis of Therapeutics. 12th ed. New York, NY: McGraw-Hill; 2011:3-16.
20. Berthold C. Enteral sedation: safety, efficacy, and controversy. Compend Cont Educ Dent. 2007;28(5):264-272.
21. Gillin JC. The long and short of sleeping pills. N Engl J Med. 1991;324(24):1735-1737.
22. Vuori E, Klaukka T. Triazolam and violent deaths. Lancet. 1992;339(8794):676-677.
23. Medawar C, Rassaby E. Triazolam overdose, alcohol and manslaughter. Lancet. 1991;338(8781):1515-1516.
24. Upjohn’s Halcion is safe and effective as currently labeled, advisory committee concludes. F-D-C Reports. 1992;May 25:9-10.
25. Upjohn’s Halcion: ‘No further action’ will be taken by FDA. F-D-C Reports. 1992; November 30:T&G-3.
26. Buxton ILO, Benet LZ. Pharmacokinetics: The dynamics of drug absorption, distribution, metabolism and elimination. In: Brunton L, Chabner B, Knollman B, eds. Goodman and Gilman’s The Pharmacological Basis of Therapeutics. McGraw Hill, New York, NY; 20-24.
27. Goodchild JH, Dickinson SC. Anxiolysis in dental practice: a report of three cases. Gen Dent. 2004;52(3)264-269.
28. Quarnstrom FW, Donaldson M. Triazolam use in the dental setting: a report of 270 uses over 15 years. Gen Dent. 2004;52(6)496-501.
29. Feck AS, Goodchild JH. Rehabilitation of a fearful dental patient with oral sedation: utilizing the incremental oral administration technique. Gen Dent. 2005; 53(1)22-26.
30. Goodchild JH, Donaldson M. Calculating and justifying total anxiolytic doses of medications for in-office use. Gen Dent. 2006;54(1):54-57.
31. Donaldson M, Goodchild JH. Maximum cumulative doses of sedation medications for in-office use. Gen Dent. 2007;55(2):143-148.
32. Gordon SM, Shimizu N, Shlash D, Dionne RA. Evidence of safety for individualized dosing of enteral sedation. Gen Dent. 2007;55(5):410-415.
33. Bennett JD, Kramer KJ, Bosack RC. How safe is deep sedation or general anesthesia while providing dental care? J Am Dent Assoc. 2015;146(9):705-708.
34. Saxen MA, Urman RD, Yepes JF, et al. A comparison of office-based anesthesia provided by dentist anesthesiologists to operating room anesthesia using national registry outcomes. Anesth Progress. In press.
35. Anesthesia Quality Institute. National Anesthesia Clinical Outcomes Registry (NACOR). https://www.aqihq.org/introduction-tonacor.aspx. Accessed July 23, 2016.
36. Society for Ambulatory Anesthesia (SAMBA). SAMBA Clinical Outcomes Registry. https://www.sambahq.org/p/cm/ld/fid=37. Accessed July 23, 2016.
37. Sweet K, Hicks V, Blackstock B. Patients may be waking up to sedation risks. Inside Medical Liability. 2016;21-25.
About the Author
Raymond A. Dionne, DDS, PhD
Faculty
Department of Pharmacology and Toxicology
Brody School of Medicine, and Department of Foundational Sciences
School of Dental Medicine
East Carolina University
Greenville, North Carolina