Flexible Phosphor Sensors: A Digital Supplement or Option to Rigid Sensors
Howard S. Glazer, DDS, FAGD
Abstract: An increasing number of dental practices are upgrading from film radiography to digital radiography, for reasons that include faster image processing, easier image access, better patient education, enhanced data storage, and improved office productivity. Most practices that have converted to digital technology use rigid, or direct, sensors. Another digital option is flexible phosphor sensors, also called indirect sensors or phosphor storage plates (PSPs). Flexible phosphor sensors can be advantageous for use with certain patients who may be averse to direct sensors, and they can deliver a larger image area. Additionally, sensor cost for replacement PSPs is considerably lower than for hard sensors. As such, flexible phosphor sensors appear to be a viable supplement or option to direct sensors.
Digital technology is unquestionably playing a significant role in the modern dental practice. One could argue that nowhere is its impact greater than in the area of radiography. There are a number of reasons why dental practices are increasingly making the conversion from film to digital radiography. Perhaps first and foremost is better image resolution. Digital radiography’s image resolution is superior to film primarily because of the ability to view the image on a large computer monitor, allowing for better diagnosis and patient education.1 Another prime advantage is faster processing. While it can take 10 to 12 minutes to complete a full-mouth series using film, digital sensors require a fraction of that time.2 Better diagnostics are also available with digital sensors, as they increase accuracy and convenience by allowing the clinician to adjust the brightness, contrast, gray scale, size, and sharpness of the image.3-5
Clinicians can also better educate their patients with digital radiography. In general, patients can more easily understand a problem when they are able to see it, and with digital radiography images can be magnified to demonstrate to the patient what the specific problem is; moreover, the image can be annotated.3 There is also less radiation exposure than with film radiography.6,7
Other benefits of using digital radiography include lower costs, as a practice is able to eliminate the expense of chemicals and chemical disposal fees, which typically would be far greater than the cost of disposable sleeves for the digital plates. It is also more ecologically friendly to the environment.2,5 Additionally, greater productivity and space efficiency can result from converting to digital, as eliminating film radiography eradicates the need for regular maintenance of the chemical processor—a major productivity-sapping task2,5—and it also frees up the office space that had been occupied by the chemical processor, chemical bottles, and file cabinets containing the film x-rays.5
Faster image access is another key advantage. Accessing a digital radiograph is done simply with the click of a mouse, as opposed to a film radiograph, which must be manually retrieved from a physical file cabinet. This can result in more efficient recordkeeping. Digital images can also be reviewed from a remote computer/location, or easily sent to other clinicians or insurance companies at any time.5,8,9
Additionally, digital imaging can result in better referrals. Images can be transmitted to a specialist to whom the practice is referring a patient, or simultaneous consultations can be made by all parties viewing the radiographic image while the patient is in the treatment room.
Lastly, if, as is widely expected, the US federal government mandates that all dental and medical practices must store their patient data digitally, practices that use digital rather than film radiography will be in full regulatory compliance.5
Direct Sensors: the Popular Option
The majority of practices employing digital radiography have opted for rigid digital sensors. Rigid sensors are sometimes called “direct” or “wired” sensors because they are connected directly to a computer. The primary advantage of this feature is that images are available to the clinician almost instantaneously. This is of particular benefit when performing endodontic procedures, which usually require a number of films at various stages (eg, canal measurement, fitting of master point, final fill, etc). A disadvantage is that each operatory utilizing these sensors must be equipped with a computer.2
Direct sensors can also be uncomfortable for patients, particularly those with small mouths, large tori, gag reflexes, or the inability to open their mouths wide.2,5 Another limitation is the fact that direct sensors are not available in all of the sizes that are available with film.5
Flexible Phosphor Sensors: An Alternative
An alternative digital radiography technology is phosphor storage plate (PSP) technology, which is increasingly being referred to as “flexible phosphor sensor” technology. Flexible phosphor sensors are wireless, non-rigid, “indirect” digital sensors—indirect in that they do not connect directly to a computer. Rather, as with film, the radiographic image is stored on the PSP in the form of a latent image. The PSP is then placed into a digital processor attached to a computer; the processor scans the PSP, digitizes the image, stores it on the computer, and displays it on the monitor, all in a matter of seconds. While this interim step means that image processing is not quite as immediate as it is with rigid, or direct, sensors, the process is significantly faster than with film.2
Flexible phosphor sensors do offer several advantages over direct sensors. For example, flexible phosphor sensors are available in the exact same sizes as film, unlike direct sensors, which have a smaller usable image area.5 Also, flexible phosphor sensors offer simpler and more convenient sensor placement. Direct sensors are more than 4-mm thick and larger than film or flexible phosphor sensors, which can make them difficult or even impossible to accurately position with patients who are unable to open their mouths wide or who have small mouths, gag reflexes, large tori, or shallow palatal vaults. With flexible phosphor sensors, practices are more likely to be able to capture 100% of the radiographs they need.5-7
Regarding patient comfort, flexible phosphor sensors are very close to conventional radiographic film size(s) and are, of course, flexible. They are smaller, softer, and thinner than rigid sensors, making them generally better able to conform to anatomical situations. Additionally, there are no cumbersome wires to be concerned about. As a result, the patient experience can be more pleasant, especially for pediatric and elderly patients.5,6
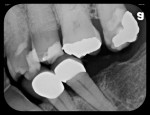
Flexible phosphor sensors generally offer a larger image area than direct sensors (Figure 1); therefore, the clinician can more accurately see and measure the complete coronal-to-apical length and obtain more mesial-distal information. In addition, the practice is less likely to miss a distal cusp or a root tip, which will save time by decreasing the number of retakes needed.2,10,11 Fewer retakes also translates to less overall radiation exposure.
Cost is another advantage with flexible phosphor sensors versus rigid sensors. Rigid sensor costs generally start at around $4,000 per sensor and can exceed $10,000 each; a dental practice will likely need more than one and perhaps several (in order to offer different sizes). Flexible phosphor sensors require the purchase of one processor, which can cost between $8,000 and $20,000; however, the processor can last for many years. Individual flexible phosphor sensors generally cost up to $40 and can often be used hundreds of times.1,5,7 Additionally, flexible phosphor sensors use the same workflow as film, which means the practice’s staff does not need to learn a new protocol when upgrading from film radiography.5,12 Lastly, dental practices often insure their rigid sensors due to the high purchase price and the fact that the wires can potentially get in the way and lead to accidental damage. Because of the low cost and wireless nature of flexible phosphor sensors, insurance is rendered unnecessary.
Ultra-Compact Chairside Options
As noted earlier, the fact that flexible phosphor sensors require the use of a processor because they are not directly connected to the operatory computer means that image processing, while significantly faster than with film, is not quite as fast as with rigid, or direct, sensors. To minimize this drawback, ultra-compact, lower-priced processors have been designed for chairside use that allows an image to appear on the operatory monitor in as little as 9 seconds. An example is the ScanX® Swift (Air Techniques, www.airtechniques.com) (Figure 2). Adding an ultra-compact flexible phosphor sensor processor could be advisable for several types of practices, including:
General practitioners (GPs) in large practices who need a complementary unit for diagnosing emergencies or for when their primary radiography unit—whether it be rigid sensor, film, or flexible phosphor sensor—is in use.
GPs who provide implant, endodontic, and oral surgical procedures and who need to constantly be taking radiographs throughout their procedures without having to walk back and forth from the operatory to process the images. While these types of practices may opt for a rigid sensor due to its nearly instantaneous image processing, the chairside ultra-compact flexible phosphor sensor unit may be an option to consider given that it offers the advantages described above and takes only a matter of seconds to deliver each image to the operatory monitor.
Specialists such as oral surgeons, endodontists, and pediatric dentists who are typically taking no more than four bitewings rather than a full-mouth series.
Even a practice that is currently utilizing rigid sensors could benefit from the addition of an ultra-compact flexible phosphor sensor processor. Having “digital redundancy” gives the practice a digital option in the event of a patient whose small mouth, large tori, gag reflex, or inability to open wide makes it difficult or impossible to use a rigid sensor, or if a rigid sensor becomes damaged and unavailable for use.1,5 For general practices that are providing endodontic or implant services and typically need to be constantly taking radiographs during a root canal or implant procedure, or for specialists who normally work on one or two teeth per procedure, investing in a large flexible phosphor sensor processing unit designed for a full-mouth series of radiographs and which must be placed in a central location may not make sense. However, an ultra-compact, highly mobile, lower-priced unit may well be capable of handling their radiography needs. It may also be designed for quick and convenient feeding of the sensors into the chairside processing unit.
Clinical Examples
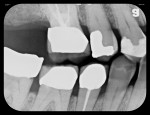
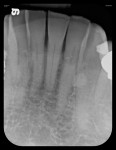
A 78-year-old male patient presented with a history of oral cancer of the right parotid gland that necessitated its removal more than 25 years ago. This resulted in severely restricting the patient’s ability to open wide on his right side (Figure 3). Consequently, it would be difficult, if not impossible, to use a rigid sensor to capture radiographs with this patient. Instead, a flexible phosphor sensor was used to capture the necessary images of the patient’s dentition with no difficulty or discomfort (Figure 4 through Figure 8).
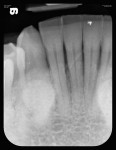
In another case, a 56-year-old man presented with severe bilateral mandibular tori (Figure 9) that made it impossible to take a radiograph using a rigid sensor that captured the entire tooth being evaluated. A flexible phosphor sensor, however, fit the patient’s anatomy with no difficulty or patient discomfort, and a radiograph was easily taken (Figure 10).
Conclusion
The benefits of upgrading from film to digital radiography—particularly better image resolution, faster image processing, faster image access, better patient education, and greater office space efficiency—can collectively have a profound impact on a practice’s productivity.10 While rigid, or direct, sensors are the most popular digital choice for practices today, flexible phosphor sensors may be a viable option for many practices. Their image processing speed, though not as immediate as rigid sensors, is much faster than film radiography. Additionally, they can often comfortably accommodate patients who cannot tolerate rigid sensors. Moreover, they provide a larger image area that is more likely to capture the entire apex and can be more economical than rigid sensors. A clinician might also consider “digital redundancy” whereby the practice utilizes both rigid and flexible phosphor sensors.
Disclosure
The author has no financial interest in any of the companies mentioned in this article.
About The Author
Howard S. Glazer, DDS, FAGD
Private Practice, Fort Lee, New Jersey; Fellow and Past President, Academy of General Dentistry; Former Assistant Clinical Professor in Dentistry, Albert Einstein College of Medicine, Bronx, New York
References
1. Jablow M. Digital radiography: analyzing the benefits. Compend Contin Educ Dent. 2012;33(2):142-143.
2. Cederberg RA, Jaquith P. Implementing dental digital radiography into a dental practice. Sidekick Web site. https://sidekickmag.com/technology/implementing-digital-radiography-into-a-dental-practice/. Accessed April 3, 2014.
3. van der Stelt PF. Better imaging: the advantages of digital radiography. J Am Dent Assoc. 2008;139(suppl):7S-13S.
4. van der Stelt PF. Filmless imaging: the uses of digital radiography in dental practice. J Am Dent Assoc. 2005;136(10):1379-1387.
5. Benjamin S. Phosphor plate radiography: an integral component of the filmless practice. Dent Today. 2010;29(11):89.
6. Strassler HE, Singhal V. Digital radiography for the allied dental professional. Inside Dental Assisting. 2012;8(2):30-37.
7. Watson JA. A perspective on digital radiography. Inside Dentistry. 2011;7(6):100-104.
8. Kantor ML. Dental digital radiography: more than a fad, less than a revolution. J Am Dent Assoc. 2005;136(10):1358-1362.
9. Christensen GJ. Why switch to digital radiography? J Am Dent Assoc. 2004;135(10):1437-1439.
10. Kouzoukian JG. Flexible phosphor sensors: the apex of digital radiography. Inside Dentistry. 2014;10(4):90.
11. Freedman G. Wireless digital sensors. Oral Health. July 2013:28-32.
12. Jablow M. Implementing digital radiography into your practice. Inside Dentistry. 2008;4(3):88-90.