Achieving Esthetic Success While Avoiding Extensive Tooth Reduction
Abstract: This case report demonstrates the importance of both careful diagnosis and thorough patient education when planning treatment for a worn and actively chipping dentition. At presentation, the patient had assumed that porcelain crowns would be needed to restore her teeth. Historically, her wear had been attributed to nocturnal bruxism. However, after a diagnostic work-up, her attrition was determined to be the result of an aberrant tooth position, which resulted in a constricted envelope of function. This diagnosis provided the opportunity to orthodontically reposition the teeth, and then achieve normal function and esthetic success with either indirect porcelain adhesively retained or additive direct resin restorations instead of more invasive, cohesively retained porcelain crowns. During orthodontic treatment, the teeth were restored with direct resin. No further restorative treatment was needed. This case has been successful for more than 6 years post-treatment, without the use of a protective appliance.
Excessive tooth wear can result from teeth being “in the way” during normal function, as well as from parafunctional habits. A successful treatment plan requires the foundation of a thorough assessment and subsequent accurate diagnosis.
In this case, a woman presented with concerns regarding the worsening wear on her front teeth. She reported that her teeth were becoming shorter and the biting edges were chipping. An examination and diagnosis determined that the wear was caused by tooth-position interferences during normal mastication. It was demonstrated to the patient that a significant amount of tooth structure loss would be necessary to restore her teeth with porcelain restorations in their current position. Once the patient understood the long-term benefits of preserving tooth structure, she ultimately agreed to orthodontic repositioning. A more conservative treatment plan was implemented, thereby reducing the lifelong biomechanical risk to the patient’s dentition.
Clinical Case Overview
A 48-year-old female patient presented with concerns about current chipping and “wearing away” of her incisors1 (Figure 1 and Figure 2). Upon questioning, she said she did not believe she had bruxism, but acknowledged she might be clenching. Her dental history included a recent root canal treatment on tooth No. 14, followed by extraction of the tooth. Her previous dental provider recommended “braces” to correct the chipping problem, and the oral surgeon who had recently removed tooth No. 14 suggested an implant. The medical history was noncontributory.
Diagnostic Findings, Risk Assessment, and Prognosis
Periodontal: The periodontal examination revealed four sites of 4 mm, all others being 3 mm or less, with only localized and light bleeding. No mobility or furcation involvements were noted. Findings from radiographic analysis revealed localized slight bone loss, indicating AAP type II.
Risk: Low
Prognosis: Good
Biomechanical: The patient had third molars electively removed at age 20, and no caries was observed. Tooth No. 14 had been missing for approximately 1 year, despite endodontic treatment. Structural compromise was observed in teeth Nos. 3, 19, and 30 due to the large existing restorations (Figure 3 and Figure 4). The amalgam restoration for tooth No. 3 was fractured, necessitating replacement.
Risk: Moderate
Prognosis: Fair
Functional: The masseter and temporalis muscles were comfortable on palpation. Both temporomandibular joints accepted loading without discomfort, and the range of motion was normal. Although the patient self-reported a clicking sound in one of her joints, no such observation could be made during the examination. Anterior tooth coupling and guidance were present, with 1 mm to 2 mm of wear noted on the anterior teeth, primarily on the facial of the lower incisors (Figure 5) and the lingual of the upper incisors (Figure 6). No wear was noted on the posterior teeth. The patient had consistently worn a full-coverage maxillary occlusal splint at night for 2 years. No wear marks were observed on the appliance, ruling out sleep bruxism.2-4 The location of wear on the facial inclines of the lower teeth and the lingual inclines of the upper teeth, combined with minimal wear of posterior teeth, indicated a constricted chewing pattern. This condition is common in patients with high interincisal angles and minimal overjet5 (Figure 7).
Risk: Moderate
Prognosis: Poor
Dentofacial: When the patient’s lips were in repose, 3 mm of incisal edge was displayed in both arches, while her full smile showed the interdental papilla but not the gingival zeniths of her anterior teeth. This observation was consistent with a diagnosis of moderate lip dynamics and tooth display (Figure 8). Incisal edges in both arches were noted to be irregular, as well as nonharmonious in the face with a retroclined appearance. Rotations and overlapped tooth positions were present, and the teeth exhibited significant shade variation, as well as translucent incisal edges of the upper incisors.
Risk: Moderate
Prognosis: Fair
Treatment Goals
Treatment goals included the following:
- adequately restore tooth No. 3 with a core-supported restoration
- lower the functional risk to the anterior teeth by repositioning the teeth in a position harmonious with the envelope of function
- increase and manage function of the posterior teeth with replacement of the missing upper left first molar, No. 14
- lower the biomechanical risk by restoring the lost tooth structure of anterior teeth first with directly bonded composite resin, thus preventing further attrition, abrasion, or erosion to the exposed dentin,6 to be followed by fabrication of adhesively retained porcelain restorations
Treatment Plan
Initially, the patient was not ready to consider orthodontics as part of her treatment plan. However, using mounted models, it was made evident that 3 mm of maxillary tooth structure would need to be removed if the teeth were to be restored in their current position, thus necessitating cohesively retained restorations. By preparing the teeth on the mounted models, the clinician enabled the patient to visualize the approximate size of the final preparations (Figure 9 and Figure 10), which helped her accept orthodontic treatment.
A consultation with the orthodontist was initiated prior to patient referral to communicate the necessary tooth position changes for conservative restorative treatment. The treatment goals agreed upon were to increase overjet and decrease overbite while providing enough interocclusal space for future restorations. After orthodontic treatment completion, final porcelain restorations were to be accomplished for the anterior teeth, with implant placement and restoration for tooth No. 14.
Treatment Phases
Phase 1: Initial Prosthetics, Upper Incisor Size Determination, Preliminary Orthodontics
Tooth No. 3 required replacement of the failed restoration, and as a result of the structural compromise, it was treated with a porcelain-fused-to-high-noble-metal crown. Upon evaluating the repose and full-smile images, the mesial incisal corner of tooth No. 9 was chosen as the esthetically pleasing final incisal edge length. Minor additions of composite resin (Renamel® Microhybrid Composite Resin, Cosmedent, www.cosmedent.com) were added to both teeth Nos. 8 and 9 to recreate appropriate incisal edge anatomy, irrespective of their vertical and horizontal positions. Orthodontic treatment was then initiated on the maxillary arch with bracket placement. The upper incisors were torqued to procline the clinical crowns, creating a more favorable overjet, while the decision was made to maintain the vertical position at the mesio–incisal corner of No. 9, while advancing facially approximately 2.5 mm.
Phase 2: Transitional Restorations
Once adequate space was present for the development of the proper lower incisor lengths, the patient returned to the office for direct resin application (Renamel Microhybrid Composite Resin) to the lower incisors. Efforts were taken to recreate the estimated original size, shape, and orientation of the lower incisors to help facilitate orthodontic realignment7 (Figure 11).
Phase 3: Completion of Orthodontics
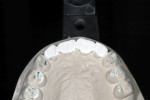
Brackets were placed on the lower arch, and final orthodontic positioning of the teeth was completed. Space for the future implant at site No. 14 was maintained during treatment (Figure 12).
Phase 4: Implant Placement, Tooth No. 14
Approximately 1 month prior to the removal of orthodontic appliances, surgical placement of the implant (Replace Select Tapered TiUnite implant, Nobel Biocare, www.nobelbiocare.com) at No. 14 was performed utilizing a two-stage approach. After orthodontic appliances were removed, second-stage surgery was completed with the placement of a healing cuff (Figure 13).
Phase 5: Final Prosthetic Restorations
With a more appropriate tooth positioning having been accomplished, the final result of direct resin bonding created an esthetic result that achieved the patient’s vision. The patient reported no more awareness of clenching, which indicated that the occlusion was now acceptable. Recognizing this as both a functional and esthetically acceptable result, the replacement of the missing molar was then initiated. After the final abutment-retained restoration for tooth No. 14 was placed, it was decided to delay fabricating porcelain restorations for the anterior teeth because the patient was satisfied with the existing composite resin restorations.
Discussion and Conclusion
Many adults are hesitant to proceed with orthodontic therapy due to the length of treatment and the unsightliness of braces. In this case, the study-cast demonstration of the amount of tooth reduction required for a prosthetic-only solution to treat the patient’s incisal wear helped communicate to her the benefit of properly positioning the teeth before placing final restorations. Upon recognizing the additional risk to her teeth, the patient decided that the orthodontic treatment was in her best interest.
It can be expected that a patient with adhesively retained, indirect porcelain restorations will have a better long-term prognosis than one with directly bonded resin restorations. However, if that same patient with a nonparafunctional constricted chewing pattern can have acceptable function created orthodontically, one can anticipate a better prognosis with whatever material is used to restore the teeth.
This case demonstrates reduction of the functional risk by creation of an acceptable envelope of function, as well as further management of function resulting from replacement of the missing molar. The treatment replaced the lost tooth structure, which served to lower the risk for biomechanical exposure to continued attrition and abrasion.
The results demonstrate a more than 6-year successfully treated case without the use of a protective appliance. While this case has not been converted to the initially planned indirect porcelain restorations, the templates for final prosthetics are in place (Figure 14), and taking the case to completion would be a straightforward procedure. The importance of reducing the functional risk before placement of any restorations was demonstrated by the long-term success of a restorative material with limited mechanical strength.
ACKNOWLEDGMENT
The author wishes to recognize the dedication to interdisciplinary treatment of Dan Grob, DDS, MS, Tucson, Arizona, for his orthodontic treatment; Ron Quintia, DDS, Tucson, Arizona, for his surgical talent in implant placement; and Dental Prosthetics Laboratory, Tucson, Arizona, for its laboratory expertise.
ABOUT THE AUTHOR
Douglas E. McMaster, DDS
Mentor, Kois Center, Seattle Washington; Private Practice, Tucson, Arizona
REFERENCES
1. Kois J, Hartrick N. Functional occlusion: science-driven management. Journal of Cosmetic Dentistry. 2007;23(3):54-57.
2. Harada T, Ichiki R, Tsukiyama Y, Koyano K. The effect of oral splint devices on sleep bruxism: a 6-week observation with an ambulatory electromyographic recording device. J Oral Rehabil. 2006;33(7):482-488.
3. van der Zaag J, Lobbezoo F, Wicks DJ, et al. Controlled assessment of the efficacy of occlusal stabilization splints on sleep bruxism. J Orofac Pain. 2005;19(2):151-158.
4. Lavigne GJ, Cistulli PA, Smith MT. Sleep Medicine for Dentists: A Practical Overview. Hanover Park, IL: Quintessence Publishing; 2009.
5. Kois JC. Functional Occlusion I, Course II. Seattle, WA: March 6-8, 2006.
6. Margeas R. Composite resin: a versatile, multi-purpose restorative material. Compend Contin Educ Dent. 2012;33(1):42-45.
7. Bassett J. To plan or not to plan: that is the question! Aesthetically guided transitional bonding for space management quandaries. Dent Today. 2012;31(11):128-131.