Self-Report of Latex Allergy By Patients Visiting a Dental Clinic
James Guggenheimer, DDS; Steven Barket, DMD; Marnie Oakley, DMD; and John Close, MA
Abstract
BACKGROUND: The prevalence of latex allergy among dental patients is not known, although it has been increasing in the population since 1982, when the use of gloves was expanded to prevent the transmission of infectious diseases.
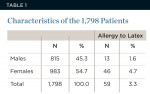
METHODS: A retrospective cross-sectional study was undertaken of 1,798 electronic health records (EHRs) of new clinic patients who registered at the University of Pittsburgh School of Dental Medicine (SDM) dental clinic between January and June 2010. Data extracted from the EHRs included age, gender, and a history of a previous latex reaction, asthma, or allergy to penicillin.
RESULTS: A previous reaction to latex was reported by 59 patients (3.3%). Women were almost three times more likely to report this (4.7% versus 1.6%, P = 0.0005). Histories of asthma or penicillin allergy in women were significantly associated with latex allergy (P = 0.0005 and P = 0.0001, respectively).
CONCLUSIONS: The reported rate of a previous reaction to latex in this patient sample was higher than that of the general population. This may, in part, be related to repeated exposures to latex-containing gloves.
CLINICAL IMPLICATIONS: Practitioners are increasingly likely to encounter patients who have had a reaction to latex. Non-latex products must be available for these patients, who are more likely to be women and individuals with asthma or an allergy to penicillin.
Hypersensitivity or allergy to latex-containing products is a relatively new phenomenon1-3 and has become an issue of increasing concern for both dental care providers and patients.4 The prevalence of latex allergy in patients receiving dental care, however, has not been determined. A comprehensive review of latex hypersensitivity was addressed by the American Dental Association Council on Scientific Affairs in 1999.4 The extent of interest in latex allergy is reflected by an increasing number of publications on this subject and the establishment, in 1991, of the self-help organization ALERT, Inc. (Allergy to Latex Education and Resource Team), which is currently known as the American Latex Allergy Association; its website (www.latexallergyresources.org) provides information on all facets of latex allergy.
The increasing likelihood of encountering patients with hypersensitivity to latex may be related to repeated exposure to the natural rubber latex protein, which is the primary mediator that is associated with the development of an allergy.5,6 This increased exposure is largely attributed to the widespread use of latex-containing gloves, one of several infection-control barriers that has been adopted in conjunction with providing many components of healthcare.5-7 The use of gloves was greatly expanded when the Centers for Disease Control focused on the prevention of transmission of the human immunodeficiency virus (HIV) in several “precautions” and “recommendations” that were published between 1982 and 1987.8-12 These guidelines specifically included dentistry in 1986.13 In addition to healthcare, other professions and occupations—such as food processing and handling, housekeeping, public safety, veterinary medicine, cosmetology, and construction—have also adopted the use of gloves.6,14
The association between repeated contact with latex and the risk for developing hypersensitivity was recognized initially in patients with spina bifida as a consequence of their having undergone frequent surgical procedures.1 Similarly, it has been shown that the number of dental students who developed a hypersensitivity to latex increased as they began to use gloves while undertaking more clinical activities during their training.15 On the other hand, avoiding exposure to latex can reduce the likelihood of developing a latex allergy.16,17
It has been estimated that more than 40,000 non-healthcare-related products contain latex, which can also sensitize or cause an allergic reaction in sensitive individuals.18 Unusual examples that have been reported include exercise sports bands19 and scuba-diving equipment.20
The prevalence of latex allergy in the general population has been estimated to be less than 1%,7,21,22 but is higher in patients with other allergies or asthma.23 A study of patients attending an allergy and asthma clinic found a positive reaction to latex based on a latex skin prick test in 7% of the patients with allergies, and an overall rate of 4.5% among the allergic and asthmatic patients.23 In healthcare workers, latex allergy prevalence rates of 5% to 15% have been reported,24-29 and 13.7% among dentists practicing in the military.30 Cross-sensitivity between latex and allergy to a number of fruits and vegetables is another factor that may contribute to an allergy to latex gloves.31,32
The authors are not aware of data regarding the prevalence of latex allergy in patients receiving dental care, but this population may also be at greater risk due to the likelihood of repeated exposure. In order to address this question, a cross-sectional study of 1,798 new patients who sought treatment at the University of Pittsburgh School of Dental Medicine (SDM) was conducted between January and June 2010.
Methods
In July 2008, the SDM implemented the use of electronic health records (EHRs) using the AxiUm software management system (Exan Corp., www.exangroup.com). The present study was initiated in January 2010 in order to enable students, faculty, and staff to acquire sufficient experience and ensure accurate and reliable data entry and retrieval. Following assurance of compliance with confidentiality guidelines, approval to access the EHRs was obtained from the University’s Institutional Review Board and the University’s Information Technology Division. Using the axiUm database, records of all new patients who registered between January 4 and June 30, 2010, for either a dental emergency or a screening examination for comprehensive care were retrieved. Records were sorted by the specified date range, emergency or screening procedure code, age, and gender. Patient names, dates of birth, and social security numbers were excluded.
The questions in the medical history used to record patients’ responses to allergies were: “Do you have any allergies (medications, latex, food, etc)?” and “Do you have or have you ever had asthma?” Affirmative answers were entered on Excel spread sheets; the frequency distribution of these responses provided the basis for data analyses. Differences and degree of association between patient characteristics and latex allergy data were determined by a P value of < 0.05 and chi square (χ2) tests for association and for differences in proportions.
Results
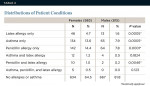
Demographics of the patients are shown in Table 1. It was initially determined that there was no significant difference in self-reported allergy to latex between the emergency and screening patients (P = 0.3211). These two groups were, therefore, combined for the subsequent data analyses. The mean age of the patients with latex allergy was 42.4 years compared with 41.4 for the non-allergic group. Patients who reported having an allergy to latex were more likely to be women (4.7% compared with 1.6% of the men, Table 2). Significantly more women than men also reported having asthma (13.6% compared with 7.9%). In addition, women were significantly more likely than men to report an allergy to penicillin (14.4% compared with 7.8%). Latex allergy, in conjunction with a history of asthma or an allergy to penicillin, was another feature that was more prevalent in women. A history of latex allergy together with asthma and a penicillin allergy was identified in five women but no men (Table 2).
Two latex-allergic patients reported that they were employed in health-related professions, although the EHRs did not record occupations. One patient, a 23-year-old man who had asthma, specifically recalled that he had a reaction to glove powder. Four of the female latex-allergic patients (6.7%) indicated that they were allergic to tomatoes, melons, or peanuts.
Discussion
Exposure to latex can result in mild to severe reactions that range from contact dermatitis to fatal anaphylaxis.5,31,33 Based on the findings from this study, 3.3% of this sample of patients who were seeking dental care had apparently experienced a previous reaction to a latex-containing product. The risk of developing a latex allergy has been shown to increase with repeated exposure to the protein that is a constituent of natural rubber latex.31,33 Evidence for this is based on studies of patients with spina bifida, the increase in reported cases of latex allergy following implementation of the CDC’s universal precautions, and the higher rate of latex allergy that has been found among workers in healthcare and other occupations that entail the use of gloves.1,6,14,24 Although there is a well-established link between latex exposure and becoming allergic, it has been suggested that the higher prevalence rates that have been observed and reported since the 1980s may, in part, be related to an increased awareness and diagnosis of latex allergy.7
The authors’ findings that women with histories of asthma or allergy to penicillin were more likely to report a latex allergy are consistent with the literature.23,31,33 In this regard, it is important to note that patients with preexisting asthma may not only be predisposed to developing a latex allergy, but are also at risk for severe reactions in the airway if they inhale aerosol that is released from powdered latex gloves.34,35 The higher rate of latex allergy that was found in patients who reported an allergy to penicillin is another recognized predisposing factor in atopic individuals, who tend to develop allergies to multiple substances over time.23,31,33 The higher prevalence of latex allergy in the women may be related to their greater likelihood for occupational exposure.14,16,33 Various fruits and vegetables have been shown to have allergic cross-reactivity with latex,31,32 and this predisposing factor was identified in four of the study’s 59 latex-allergic patients (6.8%).
This study relied on self-reports of latex allergy that were based on the patients’ having experienced a previous reaction. A history of a previous reaction to latex is a reasonable premise for establishing the diagnosis of an allergy,33,36 which can be confirmed, if necessary, by tests that employ the use of controlled exposure to latex (eg, skin prick) and/or measurement of latex-specific immunoglobulin E (IgE) antibodies.23,24,30,31,33,37 In the dental setting, however, testing patients may not be feasible, practical, or cost-effective. A history suggestive of latex allergy can be elaborated upon by several latex allergy-specific follow-up questions such as whether or not the patient has experienced any of the following: contact dermatitis or urticaria, rhinitis, wheezing or asthma, conjunctivitis, or anaphylaxis.31 Additional guidelines for the practitioner are listed in Table 3. Irrespective of the methods used to ascertain the presence of a latex allergy, all latex-containing products should be avoided when a patient reports having a previous hypersensitivity or an allergic reaction to a latex product. A variety of non-latex alternatives are now available when allergy is reported or suspected.4
The health as well as legal implications of adverse reactions to latex products during the provision of healthcare have prompted at least one major health center to transition to a “latex-safe environment.”38 The SDM has also discontinued the use of latex gloves. Although the cost of this conversion has been seen as a major obstacle,38 it has been shown that this process can be cost-effective.39
Conclusions and Clinical Implications
The results of this study suggest that patients who seek dental care may be at somewhat greater risk of having a latex allergy when compared with the general population. Since contact with latex during the provision of dental care is extremely likely given the number and diversity of latex-containing products to which the population is exposed, the dental practitioner should have an inventory of non-latex-containing supplies and materials that can be substituted when treating patients with a history of a reaction to latex.4 It may also be prudent for the practitioner to consider using alternative products, particularly when treating patients who may be at higher risk. These patients include those who are engaged in healthcare, those with asthma or who have an allergy to penicillin or other substances, as well as older, medically compromised individuals, who are likely to have had more frequent exposure to gloves and other latex-containing medical devices.
References
1. Slater JE. Rubber anaphylaxis. N Engl J Med. 1989;320(17):1126-1130.
2. Spaner D, Dolovich J, Tarlo S, et al. Hypersensitivity to natural latex. J Allergy Clin Immunol. 1983;83(6):1135-1137.
3. Taylor J, Cassettari J, Wagner W, Helm T. Contact urticaria and anaphylaxis to latex. J Am Acad Dermatol. 1989:21(4 Pt 2):874-877.
4. The dental team and latex hypersensitivity. ADA Council on Scientific Affairs. J Am Dent Assoc. 1999;130(2):257-264.
5. Turjanmaa K, Alenius H, Makinen-Kiljunen S, et al. Natural rubber latex allergy. Allergy. 1996:51(9):593-602.
6. Rolland JM, O’Hehir RE. Latex allergy: a model for therapy. Clin Exp Allergy. 2008;38(6):898-912.
7. Sussman GL, Beezhold DH. Allergy to latex rubber. Ann Intern Med. 1995;l22(1):43-46.
8. Centers for Disease Control. Acquired immune deficiency syndrome (AIDS): precautions for clinical and laboratory staffs. MMWR Morb Mortal Wkly Rep. 1982;31(43):577-580.
9. Centers for Disease Control. Acquired immunodeficiency syndrome (AIDS): precautions for health-care workers and allied professionals. MMWR Morb Mortal Wkly Rep. 1983;32(34):450-451.
10. Centers for Disease Control. Recommendations for preventing transmission of infection with human T-lymphotropic virus type III/lymphadenopathy-associated virus in the workplace. MMWR Morb Mortal Wkly Rep. 1985;34(45):681-695.
11. Centers for Disease Control. Recommendations for preventing transmission of infection with human T-lymphotropic virus type III/lymphadenopathy-associated virus during invasive procedures. MMWR Morb Mortal Wkly Rep. 1986;35(14):221-223.
12. Centers for Disease Control. Recommendations for prevention of HIV transmission in health-care settings. MMWR Morb Mortal Wkly Rep. 1987;36(Suppl 2):1-18.
13. Centers for Disease Control. Recommended infection-control practices for dentistry. MMWR Morb Mortal Wkly Rep. 1986;35(15):237-242.
14. Dillard SF, Hefflin B, Kaczmarek RG, et al. Health effects associated with medical glove use. AORN J. 2002;76(1):88-96.
15. Tarlo SM, Sussman GL, Holness DL. Latex sensitivity in dental students and staff: a cross-sectional study. J Allergy Clin Immunol. 1997;99(3):396-401.
16. Poley GE Jr, Slater JE. Latex allergy. J Allergy Clin Immunol. 2000;105(6):1054-1062.
17. Monitto CL, Hamilton RG, Levey E, et al. Genetic predisposition to natural rubber latex allergy differs between health care workers and high-risk patients. Anesth Analg. 2010;110(5):1310-1317.
18. Deval R, Ramesh V, Prasad GB, Jain AK. Natural rubber latex allergy. Indian J Dermatol Venereol Leprol. 2008;74(4):304-310.
19. Untersmayr E, Lukschal A, Hemmer W, et al. Exercise with latex sport bands represents a risk for latex allergic patients. Immunol Lett. 2008;115(2):98-104.
20. American Latex Allergy Association. Anaphylaxis during scuba diving: A hidden source of latex hypersensitivity. The ALERT Newsletter. Winter 2004;10(4). https://www.latexallergyresources.org/winter-2004-vol10-no-4. Accessed September 19, 2012.
21. American Latex Allergy Association. Latex allergy topics. Statistics. https://www.latexallergyresources.org/statistics. Accessed September 19, 2012.
22. Liss GM, Sussman GL. Latex sensitization: occupational versus general population prevalence rates. Am J Ind Med. 1999;35(2):196-200.
23. Hadjiliadis D, Khan K, Tarlo S. Skin test responses to latex in an allergy and asthma clinic. J Allergy Clin Immunol. 1995;96(3):431-432.
24. Bousquet J, Flahault A, Vandenplas O, et al. Natural rubber latex allergy among health care workers: a systematic review of the evidence. J Allergy Clin Immunol. 2006;118(2):447-454.
25. Lagier F, Vervloet D, Lhermet I, et al. Prevalence of latex allergy in operating room nurses. J Allergy Clin Immunol. 1992;90(3):319-322.
26. Settipane GA. Latex allergy: another occupational risk for physicians. Allergy Proc. 1992;13(2):79-84.
27. Arellano R, Bradley J, Sussman G. Prevalence of latex sensitization among hospital physicians occupationally exposed to latex gloves. Anesthesiology. 1992;77(5):905-908.
28. Hunt LW. The epidemiology of latex allergy in health care workers. Arch Pathol Lab Med. 1993;117(9):874-875.
29. Kaczmarek RG, Silverman BG, Gross TP, et al. Prevalence of latex-specific IgE antibodies in hospital personnel. Ann Allergy Asthma Immunol. 1996;76(1):51-56.
30. Berky ZT, Luciano WJ, James WD. Latex glove allergy: a survey of the US Army Dental Corps. JAMA. 1992;268(19):2695-2697.
31. Yunginger JW. Natural rubber latex allergy. In: Middleton’s Allergy: Principles and Practice. 7th ed. Adkinson NF Jr, Bochner BS, Busse WW, et al, eds. St. Louis, MO: Mosby Elsevier; 2008:1019-1025.
32. American Latex Allergy Association. Latex allergy topics. Cross reactive food. www.latexallergyresources.org/cross-reactive-food. Accessed September 19, 2012.
33. Warshaw EM. Latex allergy. J Am Acad Dermatol. 1998;39(1):1-24.
34. Blanc PD, Toren K. How much adult asthma can be attributed to occupational factors? Am J Med. 1999;107(6):580-587.
35. Edlich RF, Long WB III, Gubler DK, et al. Dangers of cornstarch powder on medical gloves. Seeking a solution. Ann Plast Surg. 2009;63;(1):111-115.
36. Buss ZS, Kupek E, Frode TS. Screening for latex sensitization by questionnaire: diagnostic performance in health care workers. J Investig Allergol Clin Immunol. 2008;18(1):12-16.
37. Ownby DR. Strategies for distinguishing asymptomatic latex sensitization from true occupational allergy or asthma. Ann Allergy Asthma Immunol. 2003;90(5 Suppl 2):42-46.
38. Brown RH, McAllister MA, Gundlach AM, Hamilton RG. The final steps in converting a health care organization to a latex-safe environment. Jt Comm J Qual Patient Saf. 2009;35(4):224-228.
39. Phillips VL, Goodrich MA, Sullivan TJ. Health care worker disability due to latex allergy and asthma: a cost analysis. Am J Public Health. 1999;89(7):1024-1028.
Acknowledgments
The authors thank Robert Classens for assistance with identifying and retrieving patient records.
About the Authors
James Guggenheimer, DDS
Professor
Department of Diagnostic Sciences
University of Pittsburgh School of Dental Medicine
Pittsburgh, Pennsylvania
Steven Barket, DMD
Resident
Oral and Maxillofacial Pathology
Department of Diagnostic Sciences
University of Pittsburgh School of Dental Medicine
Pittsburgh, Pennsylvania
Marnie Oakley, DMD Associate Professor
Department of Restorative Dentistry/Comprehensive Care
University of Pittsburgh School of Dental Medicine
Pittsburgh, Pennsylvania
John Close, MA
Associate Professor
Department of Dental Public Health
University of Pittsburgh School of Dental Medicine
Pittsburgh, Pennsylvania