Managing Esthetic Implant Complications
Abstract
Dental implant success today is judged not only by osseointegration but also by esthetic results. Cosmetic predictability can often be difficult to attain, and esthetic implant failures can be multifactorial. Once esthetic implant failures occur, many cannot be fully corrected. Some complications must be addressed by an interdisciplinary dental team. In this summary of case reports, surgical considerations are provided, including cases of facial asymmetry/recession due to facial implant placement or bone loss resulting from technique/treatment failures, as well as papillary deficiencies. Restorative considerations for correcting failures are also discussed.
Initially, dental implant success was defined only by osseointegration.1 That was almost 30 years ago, and today an implant is not considered successful unless the patient is pleased with both the functional and esthetic results.2,3 There is no doubt that an implant can be a successful replacement for a tooth. The cosmetic predictability, however, can be an issue.4 Esthetic implant failures can be related to many factors.5,6 Failure could be due to restorative issues with regard to form, shade, and translucency, or anatomical issues. Many complications are related more to the implant position and the associated anatomical findings.7,8 Surgically malposed implants can be catastrophic and commonly cannot be fully corrected. Restorative failures usually are less difficult to correct.9 Replacing the restorations and making the necessary corrections can be costly, but much less so than replacing implants.
Given that clinical success in the esthetic zone now includes the patient’s satisfaction with the appearance, the implant and restoration should blend as if it were a natural tooth. Objective indexes of esthetic success have been proposed to better evaluate therapeutic successes. The White Esthetic Scoring (WES) system was proposed by Belser in 2009 to assess the restoration.10 Soft-tissue indices have also been developed to assess the gingiva-papilla form. Alveolar and gingival deficiencies can make an optimal implant restoration a failure if the patient is unhappy. The gingival margin location is important, but the most difficult issue with predictability has been the interdental papilla.11 Jempt described a papilla scoring system to better determine if the papillary volume was acceptable.12 More detailed scoring systems have been proposed to analyze the soft-tissue outcome. Fürhauser first described the Pink Esthetic Scoring (PES) system in 2005.13 The PES is based on seven variables: mesial papilla, distal papilla, soft-tissue level, soft-tissue contour, alveolar process deficiency, soft-tissue color, and texture. Each variable was assessed with a 2-1-0 score, with 2 being the best and 0 being the poorest score; a perfect score would be 14. This system was simplified by Belser, with only five variables and a perfect score of 10. The WES system is similar, with five variables and 10 as a perfect score.10 In the Belser study, they evaluated 45 anterior maxillary single-tooth implants. The focus was to objectively evaluate esthetic success with the PES and WES scoring systems. The mean total was 14.7 out of a possible 20 perfect score. The range in scores varied from 11 to 18. In another study using the same scoring system, the authors found only a mean PES/WES score of 11.2.14 It is troubling to think that when implants are viewed in an objective manner, clinicians may be failing to provide their patients with predictable esthetic restorations. The numbers of esthetic failures are more likely under-reported.
The purpose of this article is to discuss many of the issues that can cause esthetic failures and how to manage these problems. Surgical corrections or restorative solutions can sometimes improve success. Frequently, interdisciplinary approaches are needed to overcome these esthetic challenges.
Esthetic Failures Caused by Malposed Implants/Improper Technique
Facial Recession and Gingival Asymmetries
Implant placement is critical. Many mistakes cannot be corrected once made. Cases 1 and 2 are examples of complications from implants placed too far facially. In the pre-maxilla, implants should be placed a minimum of 2 mm palatal to the facial contour of the adjacent teeth.15 The depth should be at least 3 mm apical to the proposed gingival margin.
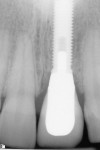
Case 1: One of the worst scenarios is an implant that is facially placed and too shallow. In Case 1, there were several factors to consider—how far facially the implant was, the diameter of the implant, and the depth of its placement. The implant was actually placed too deep (Figure 1), however this would allow for some correction. The abutment and facial emergence profile should be flat and almost concave. In this case the implant crown had been replaced and the emergence profile was kept very flat (Figure 2). The patient was informed that the ideal treatment would be explantation, grafting, and implant replacement. However, the patient refused that plan, and accepted the fact that an ideal correction in the gingival levels would not be possible.
Two subepithelial connective tissue grafts (CTG) were completed. The first graft achieved only a small improvement. Another CTG was performed 6 months later. Figure 3 shows suturing of the second CTG, which was sutured at the proposed level of the gingival margin. The flap was coronally placed to overcompensate and allow for subsequent retraction. A suspensory suture was used to coronally position the flap and was secured with composite in the contact area. The procedure was successful in placing the gingival margin in a more esthetic symmetrical location (Figure 4).
Case 2: This case involved an implant that had been placed well beyond an acceptable position to the facial (Figure 5). The facial position caused progressive recession to occur (Figure 6). The esthetic result—that the metal abutment was visible—became increasingly unacceptable to the patient over a 2-year period. The patient was informed that neither grafting nor changing the crown would achieve the desired cosmetic correction. Depth was also an issue.
Explantation was the only option offered to the patient, who was informed that at least two surgical procedures would be needed and treatment time would last approximately 1 year. The implant was explanted and the site grafted. The incision design was such that the papilla were preserved and not elevated. It should be noted that explantation can be an aggressive procedure and complications can occur; while the defect is augmented, complete regeneration of the ridge is not always fully predictable. In this case, the site was grafted with freeze-dried bone allograft (FDBA), platelet-derived growth factor (PDGF), and collagen membrane to later provide an optimal site (Figure 7).
Case 3: As is shown in this case, facial recession and esthetic deficiencies can also be caused by poor decision-making and sequencing of therapy. There must be adequate bone volume facially, even when the implant is placed in an ideal manner. Although immediate placement can be done, it is risky unless there is a medium-thick biotype. Special care should be taken in making decisions regarding immediate or delayed placement. Whenever an extraction is performed, some facial resorption will ensue.16,17 Even with a flapless approach, facial remodeling occurs. Some clinicians routinely place connective tissue grafts at the time of immediate placement to mask this resorption.18
In this case, the implant had been placed with an immediate protocol and slightly facial (Figure 8). The main complication was due to a partially missing buccal plate. The lack of gingival volume was also an issue. The patient was referred for repair of the defect. A connective tissue graft was completed, but only marginal improvement could be achieved (Figure 9).
Papillary Deficiencies
Problems with missing papilla are often considered the greatest area of soft-tissue failure with anterior implants.11 Papilla are delicate and must be preserved. The disruption of the supporting tooth and trans-septal fibers with a tooth extraction almost always causes some changes. Immediate implant placement and provisionalization can limit many of the changes. However, once the papilla has been damaged or lost, it is very difficult to regain.
The causes of papillary deficiencies are multifactorial. They include surgical trauma from the extraction, thin periodontium, triangular tooth-form, pre-existing crestal bone loss, misplaced implants too close to the adjacent tooth, and issues with adjacent implants.
Case 4: In this case involving a missing papilla, it was clear that the implants were placed too close to each other (Figure 10 and Figure 11). The patient, who had been referred for treatment to correct the deformity, was advised that the implants would need to be explanted and the ridge would require multiple osseous grafts prior to replacing the implants. Even with an optimal outcome, some papilla loss would be an issue. The option of prosthetic replacement of the papilla (pink porcelain) was also discussed, but the implants would first have to be replaced. The patient had financial limitations and did not return for treatment. She said she would pursue her legal options. This case shows how patients can be harmed by negligent care.
Case 5: This next case demonstrates how several issues can contribute to esthetic complications. The patient had been congenitally missing her maxillary lateral incisors, and had two canine-lateral incisor cantilever fixed partial dentures (FPDs) for more than 20 years. The FPDs had become discolored and had been replaced by implants—two full one-piece implants had been placed with osseous grafts. The implants were designed with the abutment and implant as one piece. The abutment could not be removed; it was designed to be first prepped, after which a conventional impression was taken to restore the implants. While this type of implant can be successful, it limits options in the event of complications.
The patient was referred to the author’s (Dr. Kinzer) office after four surgical procedures had resulted in the loss of the papilla next to the canines as well as significant facial gingival volume (Figure 12). The deformity was further complicated by the patient’s high smile line. These defects could be attributed to multiple factors. Initially the implants had been placed too close to teeth Nos. 6, 8, and 11 (Figure 13). The embrasure spaces were inadequate for papilla soft tissue. There had also been three CTGs attempted to increase the gingiva on the facial and interproximal areas. The grafts repeatedly failed and worsened the situation. The patient said she was exhausted from the surgeries and wanted to limit any further treatment. Many options were discussed, including removing the implants. Due to the proximity to the adjacent teeth and the potential for other complications, the patient elected to have cantilever FPDs completed again, as she had prior to the implant procedures. With the one-piece design implants, the abutments would have to be resected to submerge the implants.
Palatal pedicle connective tissue grafts were used to submerge the implants and to regain the papilla soft tissue. Previous CTGs had been performed with an envelope approach, and one had been done with acellular dermis. All previous grafts had failed. The palatal pedicle connective tissue graft is a technique that can retain a blood supply and also provide a large amount of tissue volume. The graft has been reported in the literature since 1993 when Wang et al first published on the technique.19 It has since been altered by many,20 including the current authors. The first procedure achieved great improvement in the soft-tissue contours and form.
Figure 14 shows the pedicle being flipped over the occlusal aspect of the implants. It was then placed under a split-thickness facial flap. The sites were sutured and closed, with approximately 3 mm of the grafts exposed over the resected implants (Figure 15). Figure 16 shows the facial image after the first graft; it is evident that the volume change in the papillary areas and the facial gingival level of the pontic sites are more in line with the adjacent teeth. Two other grafts were later performed. Small tunnel techniques were used on the facial, with vestibular access incisions. These grafts were meant to further increase the facial gingival volume in the pontic sites. The final intraoral view (Figure 17) shows an excellent improvement in the soft-tissue defects. The papilla volume mesial to the left canine was ideal; the right canine and central incisor still had some deficiencies. The patient refused further attempts and was happy with the outcome.
Restorative Solutions for Esthetic Correction
Given the surgical limitations that are often faced, it may be restorative dentists who can have the greatest impact on improving esthetic deficiencies. This approach mainly involves either changing materials or the design of the restoration. A common problem is the graying of the tissue facial to the implant restorations. This can result from either thin facial tissues or the use of dark/metal restorative components on the implants. Jung reported that it is not only the type of restorative material that influences color change in tissues, but it is also directly related to the thickness of the overlying tissue.21 With a mucosal thickness of 3 mm, no change in tissue color can be distinguished, regardless of material. Unfortunately, this is difficult to achieve clinically. In such situations, changing the underlying restorative material makes the most sense.
Case 6: For example, in this case the patient wanted to address the metal showing on the implant crown No. 11 and correct the darkness of the surrounding tissues (Figure 18). In order to improve the color of the tissue, this area was first addressed by augmenting the facial with connective tissue to provide increased thickness prior to changing the restoration. Ideally, the use of a custom zirconia abutment would provide the optimal improvement in tissue color. However, in this particular case, a customized metal-ceramic abutment was fabricated to remove the external presence of metal subgingivally while still providing strength. This combination of increasing the thickness of the gingiva along with changing the abutment material can prove to be effective in improving gingival esthetics (Figure 19 and Figure 20).
Case 7: Often times the required height of hard and/or soft tissue cannot be augmented to the correct position prior to implant placement, in which case it may be necessary to use some sort of prosthetic tissue replacement. In this case, a patient lost his anterior teeth due to trauma and was left with significant loss of hard/soft tissue (Figure 21). He was informed that it was not realistic to be able to obtain the correct papilla heights with conventional augmentation procedures. The use of pink ceramic or pink composite is being more widely used in dentistry to mask gingival defects.22-24 Generally, this option can work extremely well if the lip does not move high enough to show the border where the prosthetic pink meets the patient’s natural tissue (Figure 22 and Figure 23). The use of a prosthetic pink replacement material is sometimes the only way to help improve the esthetics of implant-supported restorations if the patient refuses any other surgical procedures.
Interdisciplinary Solutions for Esthetic Correction
Many times in cases where there is papilla deficiency adjacent to an implant, the practitioner who can make the greatest impact is the orthodontist. It is well understood that the papilla height around an implant is not dictated by the position of the bone around the implant, but, rather, by the location of the bone on the adjacent tooth.
Case 8: In this example (Figure 24) the patient was unhappy with the lack of papillary height on the mesial of the implant provisional of No. 7. The reason for the lack of papilla height, as compared to the contralateral side, was the more apical location of the bone on the distal of tooth No. 8. The height above bone that the papilla can predictably hold is typically 4.5 mm.25,26 In order to improve the height of the papilla in this location, the bone on the distal of No. 8 needed to be moved coronally. The clinician who is capable of improving this situation is the orthodontist (Figure 25). As No. 8 was erupted, the bone was moved coronally, and as a direct result, the papilla height was improved (Figure 26).
Case 9: When planning for implant placement, it is important to be aware of the limitations of how much soft tissue can be supported above bone in a given clinical situation, as this will directly impact the esthetic result. In this clinical situation, the patient had a long-standing FPD replacing the central incisors. Now tired of the bridge, the patient was treated by a friend, who placed implants in the central incisor locations (Figure 27). Following implant placement, the patient was unhappy with the esthetics of the provisional (Figure 28) and sought treatment at the author’s (Dr. Butler) office for correction.
The lack of tissue height between the implants as seen in Figure 28 should come as no surprise. From the work done by Salama et al27 the height of tissue that is maintained between adjacent implants is typically 3.5 mm. The problem in this specific case is that the original ridge had been edentulous for quite some time and as a result was “flat.” Even with the implants placed 3 mm apart, the 3.5 mm of tissue height was significantly impacted by the flatness of the ridge. The treatment chosen was to augment the ridge with connective tissue using a palatal pedicle connective tissue graft approach in order to improve the soft-tissue position (Figure 29 and Figure 30). Through use of the soft-tissue ridge augmentation approximately 7 mm of tissue height above the ridge was able to be obtained (Figure 31 and Figure 32).
At this point, knowing that the average amount of tissue that can be maintained above the bone between adjacent implants is 3.5 mm—compared to being able to predictably hold 6 mm to 7 mm of tissue between pontics—it was decided that a more esthetic option would be to not use the implants to support the restorations. Instead, the edentulous area was restored with a new FPD supported by the lateral incisors (Figure 33).
Discussion and Conclusion
The cases presented show that many esthetic implant failures cannot be fully corrected. This article is not comprehensive in discussing all types of esthetic failures. Peri-implantitis has not been discussed. Bone loss from chronic inflammation can contribute to esthetic complications. Peri-implantitis can lead to significant recession and is difficult to treat.28,29 The etiology can be due to multiple factors such as pre-existing bone loss, excess cement, occlusal overload, and bacterial plaque.
To improve soft-tissue predictability, clinicians should have extensive training and know how to best manage the complications that can occur. One study showed that experience can be a significant factor with implant survival rates. The survival rate of implants placed by students in a post-graduate training program was only 84% for the first 50 implants placed.30 The percentage of implants placed after the first 50 improved to 94%. This study did not address the esthetic complications, only implants that actually osseointegrated.
Preservation is the key to success with esthetic implants. Immediate implant placement has become popular to help improve results. Immediate implant placement and immediate provisionalization can help preserve the gingival form, but there is some risk of bone loss without careful case selection. In a recent study, 8% of cases completed in this manner had >1 mm of recession.31 This small amount of recession may be related to the immediate implant protocol. The previously mentioned PES/WES scoring system was used for assessment.10 Interestingly, five of 25 (20%) cases were considered esthetic failures.
It is important that clinicians strive to improve the routine cosmetic success of dental implants. While clinicians often encourage patients to replace heavily restored teeth with dental implants based on their functional success, the esthetic outcome should be predictable to ensure patient satisfaction. Thorough treatment planning and utilization of the full interdisciplinary team can prevent many failures.
References
1. Albrektsson T, Zarb G, Worthington P, Eriksson AR. The long-term efficacy of currently used dental implants: a review and proposed criteria of success. Int J Oral Maxillofac Implants. 1986;1(1):11-25.
2. Belser U, Buser D, Higginbottom F. Consensus statements and recommended clinical procedures regarding esthetics in implant dentistry. Int J Oral Maxillofac Implants. 2004;19 suppl:73-74.
3. Smith DE, Zarb GA. Criteria for success of osseointegrated endosseous implants. J Prosthet Dent. 1989;62(5):567-572.
4. Botticelli D, Renzi A, Lindhe J, Berglundh T. Implants in fresh extraction sockets: a prospective 5-year follow-up clinical study. Clin Oral Implants Res. 2008;19(12):1226-1232.
5. Belser UC, Buser D, Hess, et al. Aesthetic implant restorations in partially edentulous patients—a critical appraisal. Periodontol 2000. 1998;17:132-150.
6. Funato A, Salama MA, Ishikawa T, et al. Timing, positioning, and sequential staging in esthetic implant therapy: a four-dimensional perspective. Int J Periodontics Restorative Dent. 2007;27(4):313-323.
7. de Lange GL. Aesthetic and prosthetic principles for single tooth implant procedures: an overview. Pract Periodontics Aesthet Dent. 1995;7(1):51-61.
8. Phillips K, Kois JC. Aesthetic peri-implant site development. The restorative connection. Dent Clin North Am. 1998;42(1):57-70.
9. Gehrke P, Degidi M, Lulay-Saad Z, Dhom G. Reproducibility of the implant crown aesthetic index—rating aesthetics of single-implant crowns and adjacent soft tissues with regard to observer dental specialization. Clin Implant Dent Relat Res. 2009;11(3):201-213.
10. Belser UC, Grutter L, Vallati F, et al. Outcome evaluation of early placed maxillary anterior single-tooth implants using objective esthetic criteria: a cross-sectional, retrospective study in 45 patients with a 2- to 4-year follow-up using pink and white esthetic scores. J Periodontol. 2009;80(1):140-151.
11. Sullivan D, Kay H, Schwarz M, Gelb D. Esthetic problems in the anterior maxilla. Int J Oral Maxillofac Implants. 1994;9(suppl):64-74.
12. Jemt T. Regeneration of gingival papillae after single-implant treatment. Int J Periodontics Restorative Dent. 1997;17(4):326-333.
13. Fürhauser R, Florescu D, Benesch T, et al. Evaluation of soft tissue around single-tooth implant crowns: the pink esthetic score. Clin Oral Implants Res. 2005;16(6):639-644.
14. Cho HL, Lee JK, Um HS, Chang BS. Esthetic evaluation of maxillary single-tooth implants in the esthetic zone. J Periodontal Implant Sci. 2010;40(4):188-193.
15. Saadoun AP, LeGall M, Touati B. Selection and ideal tridimensional implant position for soft tissue aesthetics. Pract Periodontics Aesthet Dent. 1999;11(9):1063-1072.
16. Covani U, Cornelini R, Barone A. Bucco-lingual bone remodeling around implants placed into immediate extraction sockets: a case series. J Periodontol. 2003;74(2):268-273.
17. Araújo MG, Sukekava F, Wennström JL, Lindhe J. Ridge alterations following implant placement in fresh extraction sockets: an experimental study in the dog. J Clin Periodontol. 2005;32(6):645-652.
18. Grunder U. Crestal ridge width changes when placing implants at the time of tooth extraction with and without soft tissue augmentation after a healing period of 6 months: report of 24 consecutive cases. Int J Periodontics Restorative Dent. 2011;31(1):9-17.
19. Wang PD, Pitman DP, Jans HH. Ridge augmentation using a subepithelial connective tissue pedicle graft. Pract Periodont Aesthet Dent. 1993;5(2):47-51.
20. Khoury F, Happe A. The palatal subepithelial connective tissue flap method for soft tissue management to cover maxillary defects: a clinical report. Int J Oral Maxillofac Implants. 2000;15(3):415-418.
21. Jung RE, Sailer I, Hämmerle CH, et al. In vitro color changes of soft tissues caused by restorative materials. Int J Periodontics Restorative Dent. 2007;27(3):251-257.
22. Coachman C, Salama M, Garber D, et al. Prosthetic gingival reconstruction in a fixed partial restoration. Part 1: introduction to artificial gingiva as an alternative therapy. Int J Periodontics Restorative Dent. 2009;29(5):471-477.
23. Salama M, Coachman C, Garber D, et al. Prosthetic gingival reconstruction in the fixed partial restoration. Part 2: diagnosis and treatment planning. Int J Periodontics Restorative Dent. 2009;29(6):573-581.
24. Small BW. The use of pink porcelain for gingival defects in restorative dentistry: a case report. Gen Dent. 2010;58(4):285-287.
25. Tarnow DP, Magner AW, Fletcher P. The effect of the distance from the contact point to the crest of bone on the presence or absence of the interproximal dental papilla. J Periodontal. 1992;63(12):
995-996.
26. van der Veldon U. Regeneration of the interdental soft tissues following denudation procedures. J Clin Periodontal. 1982;9(6):455-459.
27. Salama M, Ishikawa T, Salama H, et al. Advantages of the root submergence technique for pontic site development in esthetic implant therapy. Int J Periodontics Restorative Dent. 2007;27(6):
521-527.
28. Romanos G, Ko HH, Froum S, Tarnow D. The use of CO(2) laser in the treatment of peri-implantitis. Photomed Laser Surg. 2009;27(3):381-386.
29. Renvert S, Polyzosis I, Maguire R. Re-osseointegration on previously contaminated surfaces: a systematic review. Clin Oral Implants Res. 2009;20(suppl 4):216-227.
30. Zoghbi SA, de Lima LA, Saraiva L, Romito GA. Surgical experience influences 2-stage implant osseointegration. J Oral Maxillofac Surg. 2011;69(11):2771-2776.
31. Cosyn J, Eghbali A, De Bruyn H, et al. Immediate single-tooth implants in the anterior maxilla: 3-year results of a case series on hard and soft tissue response and aesthetics. J Clin Periodontol. 2011;38(8):746-753.
About the Authors
Bobby Butler, DDS
Affiliate Faculty Member
University of Washington School of Dentistry
Seattle, Washington;
Private Practice
Seattle, Washington
Greggory A. Kinzer, DDS, MSD
Faculty
Spear Education at the Scottsdale Center for Dentistry
Scottsdale, Arizona
Private Practice
Seattle, Washington