Overcoming Unforeseen Incidents: What to do When an Unlikely Event Occurs
Abstract
Despite clinicians’ best efforts, throughout the course of practicing dentistry on a daily basis unforeseen incidents are sometimes unavoidable. While these unexpected events can initially be upsetting to both the patient and the clinician, it is paramount that the clinician maintain composure and calmly rectify the potentially damaging situation. This case report describes an incident in which the clinician’s equipment malfunctioned while performing root canal therapy on a patient, and how the clinician was able to carefully dislodge a broken instrument from the patient’s mid-root while avoiding perforation of the tooth.
While practicing dentistry on an everyday basis, there may be times when clinicians encounter unforeseen, problematic events such as an equipment malfunction. If not handled properly such incidents can be traumatic to the patient and detrimental to the clinician’s practice. Planning and preparation are essential to overcoming such potentially challenging situations. The following case depicts an instance in which the author’s instrumentation failed while performing root canal therapy on a patient, and the steps that were taken to rectify the problem.
Case Report
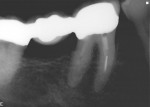
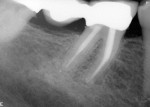
A 75-year-old man was referred to the author’s office for examination of tooth No. 30 for possible root canal therapy. He had recently been experiencing discomfort with hot and cold foods and was having slight pain chewing on his lower right side. A bridge from Nos. 30 through 32 had been permanently cemented within the previous year (Figure 1). The patient’s medical history was non-contributory. He did, however, demonstrate a significant, constant tremor, and the author surmised that this could impede his ability to treat the patient if root canal therapy was indeed necessary.
Diagnosis of the etiology of the patient’s pain began by testing his teeth to percussion, and it was evident that only tooth No. 30 was painful to tapping. Next, the lower right quadrant was tested with Hygenic® Endo-Ice® (Coltène-Whaledent, www.coltene.com). The results were positive, with non-lingering responses on teeth Nos. 29 and 32. By testing the “normal” teeth first, a clinician is able to determine a patient’s baseline response. For some people, slight lingering to cold may be normal, while for others it may not be. After then testing the tooth in question, No. 30, it was quite apparent that this was the source of the patient’s pain. He felt acute pain that lingered for almost 1 minute, allowing the author to diagnose the condition as irreversible pulpitis, No. 30, with acute periradicular periodontitis.
Having reviewed all treatment modalities, alternatives, risks, and benefits, it was determined that root canal therapy on tooth No. 30 would be performed. Whenever clinicians treat patients, they must be aware that complications may occur, especially in retreatment cases. But even for nonsurgical root canal therapy, anatomy may impede a clinician’s attempt to successfully negotiate the canals. Therefore, by under-promising and over-delivering, clinicians can improve the patient’s overall satisfaction.
Treatment began by giving the patient an inferior alveolar block with 1.8 ml mepivicaine and 0.9 ml 2% lidocaine with epinephrine 1:100,000. This was followed by a long buccal injection, administering 0.9 ml of 2% lidocaine with epinephrine 1:100,000. Parirokh et al demonstrated that combining an inferior alveolar block with a long buccal infiltration injection provided more effective anesthesia in mandibular molars with irreversible pulpitis.1
Some clinicians prefer to give ibuprofen to patients preoperatively to help them achieve better anesthesia for an inflamed tooth, but support from the literature is mixed. Aggarwal et al recently demonstrated that preoperative administration of ibuprofen or ketorolac had no significant effect on the success rate of inferior alveolar nerve block in patients with irreversible pulpitis.2 Oleson et al further confirmed that for mandibular posterior teeth, a dose of 800 mg of ibuprofen given 45 minutes before the administration of an inferior alveolar block did not result in a statistically significant increase in anesthetic success in patients with irreversible pulpitis.3 Meanwhile, Parirokh et al found that premedication with ibuprofen and indomethacin significantly increased the success rates of inferior alveolar block anesthesia for teeth with irreversible pulpitis.4
In this particular case, having visited his restorative dentist prior to treatment, the patient had already been given a 600 mg dose of ibuprofen. Nevertheless, the author does not routinely prescribe that, but instead uses other methods of injection to alleviate pain, such as periodontal ligament (PDL) or intraosseous. In rare cases, the author may have to resort to an intrapulpal injection, but only very infrequently. This is because of a strategy of often waiting 15 minutes after administering a block to begin treatment and because in the author’s practice, more necrotic teeth and retreatments of prior root canal therapies are treated than teeth with irreversible pulpitis.
After waiting 15 minutes, tooth No. 30 was again tested to Hygenic Endo-Ice to see if pulpal anesthesia was achieved. The patient felt no pain, so the procedure was started. The tooth was isolated with a rubber dam and access preparation began using a No. 2 round diamond bur to remove the occlusal porcelain, allowing the metal coping underneath to be visible. With the aid of a microscope, access preparation was continued using a straight metal-cutting bur. The pulp was inflamed, and bleeding was immediately visible in the chamber. While this confirmed the diagnosis, it also posed some problems.
Naturally, proper magnification and a clear operating field is necessary to achieve good visibility inside a crown. This can be challenging when a tooth is inflamed. In this case, the problem was solved by locating the orifices with a 10 and 15 .02 hand file and locating the canals first. This was done without using the instrument beyond resistance. Then a 30 tip, .04 taper rotary file was used to clean out the coronal or mid-root portion of the canals. This allowed for better visualization of the orifices and removed enough coronal tissue so that the bleeding began to subside. Copious irrigation with 6% (full strength) sodium hypochlorite further ensured that tissue dissolution would take place. Recent studies have demonstrated that tissue dissolution increased almost linearly as concentration of sodium hypochlorite increased.5 Also, sodium hypochlorite has been shown to eliminate Enterococcus faecalis-contaminated dentin when used in higher concentration for 40 minutes.6
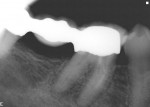
Next, canal lengths were verified with an apex locator. In this particular case, three canals were found. Having taken a 20 tip, .02 hand file to length on all three separate canals, the author was prepared to open the orifices with a No. 3 Gates Glidden drill (DENTSPLY/Caulk, www.caulk.com), allowing for better straight-line access. This is when the equipment malfunction occurred. Whether it was the patient’s constant movement, an over-aggressive technique, or inherent weakness in the bur itself, after the Gates was removed from the canal the tip of it was missing (Figure 2). Immediately it was realized that something was clearly wrong, as Gates drills are supposed to separate near the shank, not at the tip.
The author explained the situation to the patient, saying that while attempting to clean out the inflamed tissue an instrument became separated within one of the canals, and that he was hopeful to be able to retrieve it and complete the treatment successfully. The author further explained that if the broken instrument could not be retrieved, future surgery (apicoectomy) or extraction may be necessary. After the patient accepted this explanation, the arduous task of removing the Gates Glidden instrument from mid-root began, while simultaneously carefully trying not to perforate the patient’s tooth.
Correcting the Problem
To remove the Gates, several ultrasonic tips were initially used to advance down the canal, starting with larger tips (ProUltra® Endo Coated Instruments #2 and #3, DENTSPLY Tulsa Dental, www.tulsadental.com) and, finally, an ultra-fine tip (ProUltra® Endo Coated Instrument #5, DENTSPLY Tulsa Dental) set on the lowest power setting to trough away tooth structure surrounding the broken instrument. A lower setting was also used on a Mini Endo II ultrasonic unit (SybronEndo, www.sybronendo.com) for two reasons. First, with a higher power setting there is a potential to significantly gouge a tooth, thereby removing sound tooth structure. Second, the ultra-fine tip would almost certainly break at a higher setting.
Clifford J. Ruddle, DDS, recommends using a Gates to create a “platform” to begin accessing a broken instrument or bur.7 However, this can just as readily be performed with the use of ultrasonics and copious water. Having removed some tooth structure, the author could now better visualize the broken bur under a microscope.
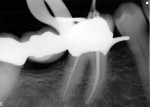
Even though enough tooth structure was removed to better visualize the top half of the broken Gates, a periapical (PA) radiograph was taken for better visualization within the canal. This additional step was invaluable, as it helped the author visualize if he was properly centered over the instrument, or if he was closer to perforating the tooth from the mesial aspect. Once it was apparent that it was permissible to proceed, the author continued to use the ultrasonic on a low power setting. Normally, without using constant water, too much heat would be generated in the periodontal ligament and tissue sloughing could result. Due to the delicate nature of this procedure, the water could not be used in combination with the ultrasonic vibration. Rather, intermittently irrigating with either water or sodium hypochlorite would reduce the chance that any heat generated by the ultrasonic tip would impact the patient’s adjacent gingiva or bone. It also allowed for better canal visibility, as there was less need to constantly dry the canal. At the end of the first visit, calcium hydroxide was placed and the tooth was sealed with cotton and Cavit™ (3M ESPE, www.3MESPE.com) (Figure 3).
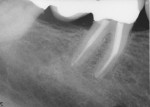
At the second visit, the patient was asymptomatic. The same amount of anesthesia was administered as at the initial visit and treatment continued. After 30 minutes of ultrasonic vibration on the lowest power setting, the broken Gates finally emerged and entered the pulp chamber where the author was able to easily remove it with a pair of college pliers. A radiograph was taken to confirm that the entire segment was removed (Figure 4). At this point, the author checked to see if any perforation had occurred mid-root. Also, completing this case would still be challenging. In fact, negotiating the mesiobuccal (MB) and mesiolingual (ML) canals was almost as arduous as removing the Gates itself. But having instrumented each to a 30 tip, .02 taper hand file, the author again medicated the patient’s tooth with calcium hydroxide and sealed the access with cotton and Cavit (Figure 5). Calcium hydroxide was placed to both medicate and confirm that no perforation had occurred. However, under the microscope, the author was able to surmise that perforation likely did not occur since no bleeding was present. In addition, because it took approximately 30 minutes to remove the Gates, the patient was brought back for a third visit to complete treatment.
At that visit, instrumentation was completed with nickel titanium rotary files to a 40 tip, .04 taper on the distal and a 35 tip, .04 taper on the mesial canals (Figure 6). While the author usually opens teeth to greater apical sizes, it was not prudent to do so in this particular case because of the curvature of the roots and the narrowness of the canals. As Donald E. Arens, DDS, once said, “the enemy of good is better” (personal communication, August 2005); that seemed to be prudent advice in this case.
Despite being treated on three separate occasions, the patient stated that he experienced little to no pain during each procedure and immediately thereafter. This is congruent with recent literature that suggests there is no significant difference in postoperative pain after single-visit or multiple-visit root canal therapy.8 Also, recent literature suggests that the combination of acetaminophen and ibuprofen may be more effective than ibuprofen alone for managing postoperative endodontic pain.9 The author routinely recommends that combination of drugs over narcotics for most healthy patients requiring root canal therapy.
Conclusion
With the patient’s root canal therapy completed, the access cavity was sealed with a composite resin restoration. At the 6-month and 1-year check-up appointments, the patient remained asymptomatic, and it appeared that everything was healing well (Figure 7 and Figure 8). No visible breakdown of lamina dura was apparent.
References
1. Parirokh M, Satvati SA, Sharifi R, et al. Efficacy of combining a buccal infiltration with an inferior alveolar nerve block for mandibular molars with irreversible pulpitis. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2010;109(3):468-473.
2. Aggarwal V, Singla M, Kabi D. Comparative evaluation of effect of preoperative oral medication of ibuprofen and ketorolac on anesthetic efficacy of inferior alveolar nerve block with lidocaine in patients with irreversible pulpitis: a prospective, double-blind, randomized clinical trial. J Endod. 2010;36(3):375-378.
3. Oleson M, Drum M, Reader A, et al. Effect of preoperative ibuprofen on the success of the inferior alveolar nerve block in patients with irreversible pulpitis. J Endod. 2010;36(3):379-382.
4. Parirokh M, Ashouri R, Rekabi AR, et al. The effect of premedication with ibuprofen and indomethacin on the success of inferior alveolar nerve block for teeth with irreversible pulpitis. J Endod. 2010;36(9):1450-1454.
5. Stojicic S, Zivkovic S, Qian W, et al. Tissue dissolution by sodium hypochlorite: effect of concentration, temperature, agitation, and surfactant. J Endod. 2010;36(9):1558-1562.
6. Retamozo B, Shabahang S, Johnson N, et al. Minimum contact time and concentration of sodium hypochlorite required to eliminate Enterococcus faecalis. J Endod. 2010;36(3):520-523.
7. Ruddle CJ. Broken instrument removal. April 2007. Available at: https://www.endoruddle.com/faq.html?name=FAQRetxInstr. Accessed March 3, 2011.
8. El Mubarak AH, Abu-bakr NH, Ibrahim YE. Postoperative pain in multiple-visit and single-visit root canal treatment. J Endod. 2010;36(1):36-39.
9. Menhinick KA, Gutmann JL, Regan JD, et al. The efficacy of pain control following nonsurgical root canal treatment using ibuprofen or a combination of ibuprofen and acetaminophen in a randomized, double-blind, placebo-controlled study. Int Endod J. 2004;37(8):531-541.
About the Author
Joseph Chikvashvili, DDS
Private Practice
West Orange, New Jersey
Director of Endodontics
Newark Beth Israel Medical Center
Newark, New Jersey