Using a Nanohybrid Composite and Diode Laser to Achieve Minimally Invasive Esthetic Anterior Restorations
By Wilson J. Kwong, DMD
Abstract
Developments in material science have contributed greatly to the evolution of composites during the past several decades. Most recently, nanohybrids and nanofilled direct composites have demonstrated the advantages of previous composite generations, such as strength, low wear, and polishability, but without many of the limitations. Concurrently, soft-tissue diode lasers also are among evolving dental products that can enable clinicians to offer less invasive restorative and esthetic treatments to patients.
Since their introduction, composite materials have been used increasingly to restore anterior and posterior teeth based on their esthetic qualities and continuously improving physical characteristics.1 An additional advantage these materials present is placement with minimally invasive preparation techniques that conserve tooth structure.2
Developments in material science have contributed greatly to the evolution of composites during the past several decades. Today’s direct composite materials include microhybrids, microfills, and nanohybrids, each of which provides dental practitioners with specific clinical, functional, and esthetic benefits.3 For example, microhybrid composites are strong materials suitable for enamel and dentin replacement in functional areas as a result of their particle size and filler loading.2 Unfortunately, their polish isn’t sustained long term.2,3 Microfilled composites, on the other hand, do provide excellent polishability and life-like esthetics, but their inability to perform well in stress-bearing areas limits their indications for use to anterior teeth and cervical lesions.2,3 The most recently introduced and beneficial direct composites are nanohybrids and nanofilled. Composed of particles and fillers of diverse and nanometer size, these materials demonstrate the advantages of previous composite generations, including strength, low wear, and polishability, but without the limitations.3-5
Concurrently, soft-tissue diode lasers also are among evolving dental products that can enable clinicians to provide less invasive restorative and esthetic treatments to patients.6-8 Soft-tissue diode-laser techniques provide practitioners with the ability to precisely complete routine esthetic procedures, including gingivectomies, gingival contouring, and treatment of excessive gingival display.7-9 Additionally, soft-tissue diode lasers are helpful in facilitating caries removal when used to trough around prepared teeth, which also can result in cleaner, more accurate impressions.8,10 Overall, soft-tissue diode lasers are less invasive and traumatic to patients and the areas surrounding treatment. They promote less postoperative discomfort for the patient, less collateral damage to healthy tissue, immediate hemostasis, and less tissue charring.9,10
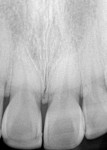
This article demonstrates the use of a soft-tissue diode laser (Odyssey® Navigator, Ivoclar Vivadent, www.ivoclarvivadent.us) in combination with a nanohybrid direct composite resin (IPS Empress Direct, Ivoclar Vivadent) to enhance the smile of a 28-year-old woman who presented with a chipped central incisor and an unbalanced excessive gingival display (Figure 1 and Figure 2). In the past, lasers would not have been considered to correct the unbalanced and excessive gingival display; only the chipped central incisor would have been addressed. However, because the patient noticed the imbalance, and the subtle soft-tissue correction could be completed in a minimally invasive way using the soft-tissue laser, the patient desired the combination of direct composite and in-office gingival treatment. She declined more aggressive treatment with indirect porcelain veneers and osseous contouring. Additionally, given the patient’s relatively young age and the overall healthy condition of her teeth, this was the most appropriate treatment plan to achieve the anticipated results.
Clinical Protocol
After the patient accepted the treatment plan involving minor gingival recontouring and direct composite bonding with minimal tooth reduction, the gingival zeniths for the central incisors were idealized by first performing gingival contouring on the preoperative model (Figure 3). Essix material was placed over the model and trimmed to expose the margins. This enabled visualization of the hard and soft tissues and provided a template for tissue removal (Figure 4).
A waxed-up model was fabricated for teeth Nos. 1.1, 1.2, 2.1, and 2.2 (note Canadian tooth numbering system). The Golden Proportion and width-to-height ratio were calculated at 78%, which was congruent to the patient’s ideal facial esthetics (Figure 5). A putty matrix (Siltek, Ivoclar Vivadent) was created to index the ideal incisal edge position and gauge how much tooth reduction would be required during the preparation (Figure 6).
An additional putty stent was fabricated to demonstrate final facial dimensions, which measured 1 mm to 2 mm in thickness for compo site layering, and placed in the mouth (Figure 7). Very minimal to almost no tooth reduction was required except for the distal facio-incisal aspect of tooth No. 2.1.
The preparations then were scrubbed using hydrogen peroxide, followed by another scrub using 0.2% chlorhexidine solution. They were rinsed with water to ensure the surface was clean after the scrubbings.
After measuring the pocket depths to ensure that the biologic width was not violated, the tissue was contoured using a soft-tissue diode laser (Odyssey® Navigator) at 0.8 Watts, continuous wave, and with air-cooling (Figure 8). The stent was then placed back in the mouth to show the amount of composite material needed to create ideal morphology and incisal edge translucency (Figure 9).
The enamel was etched for 10 seconds, after which the tooth surfaces were rinsed with copious amounts of water for 10 seconds and lightly air-dried. Bonding agent (Excite, Ivoclar Vivadent) was applied by placing three clicks from a Vivapen (Ivoclar Vivadent) onto the preparation for 5 seconds. The bonding agent was agitated, after which the surfaces were lightly air-dried using an ADEC tooth warmer. The bonding agent was light-cured for 20 seconds, followed by 10 seconds of light-curing in a circular motion at different angles.
The next steps represent a layering technique for composite placement that produces results similar to what can be achieved with ceramic, but with the simplicity and ease of chairside application. For this procedure, a light-curing, nanohybrid direct resin (IPS Empress Direct) that demonstrates exceptional handling properties was chosen so that consistent anterior esthetics similar to ceramics could be realized with the on-demand simplicity of composite.
A1 Dentin, A1 Enamel, and Trans 30 shades of the IPS Empress Direct composite were layered to mimic the optical characteristics of the patient’s natural tooth structure. This composite material features a broad range of true-to-nature dentin and enamel shades to provide accurate color matches and esthetic results. Dentin shades have a more opacious, saturated chroma that produces the basic color of the tooth from within. The translucency of the enamel shades provides a natural depth to the restoration, diffusing the color of the dentin the way natural tooth structure does. Additional gradations in translucency can be achieved using the translucent and opalescent shades.
With the stent in place, the A1 Enamel layer first was placed on the lingual of tooth No. 2.1 and the composite formed. This layer was cured for 20 seconds. Then, a layer of Trans 30 was placed at the incisal and cured for 20 seconds. A very thin layer of A1 Enamel was placed over the buccal, slightly onto the incisal, blended with a flat plastic instrument, and then cured for 20 seconds.
A brush with Heliobond (Ivoclar Vivadent) was used to drag the composite to a thin layer in order to create a highly polishable surface, after which the entire facial structure was created as a block, cured for 20 seconds, and the anatomy and line angles created. The restoration then was shaped, contoured, polished, and tested for flash with floss. After one tooth restoration was complete, the next tooth was treated (Figure 10).
Sof-Lex™ discs (3M ESPE, www.3MESPE.com), fluted carbide polishing burs (Brasseler, www.brasselerusa.com), diamond strips (Brasseler), and an integrated polishing system (Astropol, Ivoclar Vivadent), were used to shape and polish the restorations, as well as impart luster on the restoration surfaces (Figure 11). Because IPS Empress Direct is a nanohybrid composite, it retains its gloss similar to a microfill or nanofill. Restorations created with IPS Empress Direct can be polished quickly and easily as a result of the material’s even filler particle distribution. The resulting composite restorations and soft-tissue diode-laser gingival sculpting produced the idealized gingival zeniths, tooth size proportions, and symmetry (Figure 12, Figure 13, Figure 14 and Figure 15).
Conclusion
In this case, removing as little tooth structure as possible enabled the author to maintain the patient’s tooth structure in the best state possible. The use of the nanohybrid composite system enabled replication of the qualities and characteristics of dental ceramics and the chairside creation of life-like and natural looking restorations (Figure 16 and Figure 17).
The patient’s current nanohybrid direct composite restorations can be expected to last for years and, if necessary, be replaced with new composite restorations in the future. This would not have been possible if porcelain veneers were placed at this time. However, the option to place porcelain in the future still can be considered.
References
1. Minguez N, Ellacuria J, Soler JI, et al. Advances in the history of composite resins. J Hist Dent. 2003;51(3):103-105.
2. Sensi LG, Strassler HE, Webley W. Direct composite resins. Inside Dentistry. 2007;3(7):76-79.
3. LeSage BP. Aesthetic anterior composite restorations: a guide to direct placement. Dent Clin North Am. 2007;51(2):359-378.
4. Yesil ZD, Alapati S, Johnston W, Seghi RR. Evaluation of the wear resistance of new nanocomposite resin restorative materials. J Prosthet Dent. 2008;99(6):435-443.
5. Hervçs-García A, Martinez-Lozano MA, Cabanes-Vila J, et al. Composite resins. A review of the materials and clinical indications. Med Oral Patol Oral Cir Bucal. 2006;11(2):E215-E220.
6. Adams TC, Pang PK. Lasers in aesthetic dentistry. Dent Clin North Am. 2004;48(4):833-860.
7. Magid KS, Strauss RA. Laser use for esthetic soft tissue modification. Dent Clin North Am. 2007;51(2):525-545.
8. Pang P. Lasers in cosmetic dentistry. Gen Dent. 2008;56(7): 663-670.
9. Robbins JW. Differential diagnosis and treatment of excess gingival display. Pract Periodontics Aesthet Dent. 1999;11(2):265-272.
10. Mortiz A, Schoop U, Goharkhay K, et al. Treatment of periodontal pockets with a diode laser. Lasers Surg Med. 1998;22(5):302-311.
About the Author
Wilson J. Kwong, DMD
Private Practice
Vancouver, British Columbia