Periodontal Probing Systems: A Review of Available Equipment
Srinivas Sulugodu Ramachandra, MDS; Dhoom Singh Mehta, MDS; Nagarajappa Sandesh MDS; Vidya Baliga, MDS; and Janardhan Amarnath, MDS
Abstract
The periodontal pocket, one of the definitive signs of periodontal disease, is the most common parameter to be assessed by dental clinicians. Periodontal probes have been the instruments most commonly used to locate and measure these pockets. Regular use of periodontal probes in routine dental practice facilitates and increases the accuracy of the process of diagnosing the condition, formulating the treatment, and predicting the outcome of therapy. Advances in the field of periodontal probing have led to the development of probes that may help reduce errors in determining this parameter used to define the state of active periodontal disease. One such advance is the emergence of probes that purportedly assess periodontal disease activity noninvasively. The selection of periodontal probe depends on the type of dental practice: a general dental practitioner would require first- or second-generation probes, while third- through fifth-generation probes generally are used in academic and research institutions as well as specialty practices.
The periodontal pocket, one of the definitive signs of periodontal disease, is the most common parameter to be assessed by dental clinicians. One of the more reliable and convenient ways of detecting, measuring, and assessing the status of periodontal disease activity is through the use of periodontal probes.Periodontal probing permits dentists to identify sites with a history of periodontal disease or those at risk for periodontal breakdown. Described by Orban as the "eye of the operator beneath the gingival margin," periodontal probes are an essential part of a complete dental examination.1
Uses of Periodontal Probes
The word probe is derived from the Latin word Probo, which means "to test." Periodontal probes are used primarily to detect and measure periodontal pockets and clinical attachment loss. In addition, they are used to locate calculus; measure gingival recession, width of attached gingiva, and size of intraoral lesions; identify tooth and soft-tissue anomalies; locate and measure furcation involvements; and determine mucogingival relationships and bleeding tendencies.2 However, periodontal probing has its limitations. Reading errors may result from naturally occurring states, such as interference from the calculus on the tooth or root surface, the presence of an overhanging restoration, or the crown's contour. Another factor is operator error, such as incorrect angulation of the probe, the amount of pressure applied to the probe, misreading the probe, recording the data imprecisely, and miscalculating the attachment loss.3
Various factors, such as probe-tip size, angle of insertion of the probe, probing pressure, precision of probe calibration, and degree of inflammation in the underlying periodontal tissues, affect the sensitivity and reproducibility of measurements.4 Because the probe passes through the junctional epithelium into the underlying connective tissue in an inflamed gingival sulcus, readings of clinical pocket depth obtained with the periodontal probes do not normally coincide with the measurements up to the base of the pocket.4
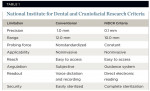
The National Institute for Dental and Craniofacial Research (NIDCR) has defined eight criteria for overcoming the limitations of conventional periodontal probing.5 Table 1 shows how conventional probing criteria has been altered by the NIDCR for this objective.
Periodontal Probe Selection and Type of Dental Practice
For consistency of use and academic purposes, in 1992, Pihlstrom et al6 classified probes into three generations. In 2000, Watts7 extended this classification by adding fourth- and fifth-generation probes. These various generations, along with their advantages and disadvantages, are in Table 2.
Various periodontal probes cater to different needs. Selecting the appropriate periodontal probe is dependent on the type of dentistry a clinician practices. The needs of a general dentist are different from those of a periodontist who usually requires a more specialized set of periodontal probes. Research facilities and academic institutions can afford and effectively use more complex and sophisticated periodontal probes. Also, because the latest generations of probes work in conjunction with computers, the state of computerization in a dental practice has to be considered during the selection process.
Periodontal probes suitable for a general dental practice:
- First-generation
- Second-generation
Periodontal probes suitable for a dental practice with an interest in periodontics:
- First-generation
- Aecond-generation
- Third-generation (if computerization is adequate)
Periodontal probes suitable for a specialty periodontal practice and university and research institutions:
- Second-generation
- Third-generation
- Fifth-generation
Periodontal Probe Generations
First-Generation (Conventional) Probes
Conventional or manual probes (Figure 1) do not control for probing pressure and are not suited for automatic data collection. These probes most commonly are used by general dental practitioners as well as periodontists. Invented in 1936 by periodontist Charles H.M. Williams, the Williams' periodontal probe is the prototype or benchmark for all first-generation probes. These probes have a thin stainless steel tip of 13 mm in length and a blunt tip end with a diameter of 1 mm. The graduations on these probes are 1 mm, 2 mm, 3 mm, 5 mm, 7 mm, 8 mm, 9 mm, and 10 mm. (The 4-mm and 6-mm markings are absent to improve visibility and avoid confusion in reading the markings.) The probe tips and handles are enclosed at 130o.8
The Community Periodontal Index of Treatment Need (CPITN) was designed by Professors George S. Beagrie and Jukka Ainamo in 1978. CPITN probes are recommended for use when screening and monitoring patients with the CPITN index. The index and its probes were first described in World Health Organization's (WHO) Epidemiology, etiology, and prevention of periodontal diseases. Report of a WHO Scientific Group.9 The FDI World Dental Federation/WHO Joint Working Group 1 has advised the manufacturers of CPITN probes to identify the instruments as CPITN–E (epidemiologic), which have 3.5-mm and 5.5-mm markings, and CPITN–C (clinical), which have 3.5-mm, 5.5-mm, 8.5-mm, and 11.5-mm markings. CPITN probes have thin handles and are lightweight (5 gm). The probes have a ball tip of 0.5 mm, with a black band between 3.5 mm and 5.5 mm, as well as black rings at 8.5 mm and 11.5 mm.
University of Michigan O probes have markings at 3 mm, 6 mm, and 8 mm. A modification of this probe with Williams' markings also is available. University of North Carolina-15 (UNC-15) probes are color-coded at every millimeter demarcation. They are the preferred probe in clinical research if conventional probes are required.
The Naber's probe is used to detect and measure the involvement of furcal areas by the periodontal disease process in multirooted teeth. Naber's probe also is used in the assessment of more complex clinical cases, including those with a restorative treatment. These probes can be color-coded or without demarcation.
Second-Generation (Constant-Pressure) Probes
The second-generation instruments are pressure sensitive, allowing for improved standardization of probing pressure. Scientific literature that demonstrated probing pressure should be standardized and not exceed 0.2 N/mm2 led to the development of their probes.10 Second-generation probes can be used in general dental practices, as well as periodontal practices, and do not require computerization in the operatory. The True Pressure Sensitive (TPS) probe (Figure 2) is the prototype for second-generation probes. Introduced by Hunter in 1994, these probes have a disposable probing head and a hemispheric probe tip with a diameter of 0.5 mm. A controlled probing pressure of 20 gm is usually applied. These probes have a visual guide and a sliding scale where two indicator lines meet at a specified pressure.11
In 1977, Armitage designed a pressure-sensitive probe holder to standardize the insertion pressure and determine how accurate probing pressure of 25 pounds affected the connective-tissue attachment.12 In 1978, van der Velden devised a pressure-sensitive probe with a cylinder and piston connected to an air-pressure system. Subsequently, it was modified with a displacement transducer for electronic pocket-depth reading.13
The electronic pressure-sensitive probe, allowing for control of insertion pressure, was introduced by Polson in 1980. This probe has a handpiece and a control base that allows the examiner to control the probing pressure. The pressure is increased until an audio signal indicates that the preset pressure has been reached.14 Polson's original design was modified by its initial users: That probe is known as the Yeaple probe, which is used in studies of dentinal hypersensitivity.15
Third-Generation (Automated) Probes
In spite of the advances in second-generation probes, other sources of errors, such as in reading the probe, recording data, and calculating attachment level, still needed to be addressed. Third-generation probes were developed to help minimize these mistakes by using not only standardized pressure, but also digital readouts of the probes' readings and computer storage of data. This generation includes computer-assisted direct data capture to reduce examiner bias and allows for greater probe precision. These probes require computerization of the dental operatory and can be used by periodontists and academic institutions for research.
The Foster-Miller probe (Foster-Miller, Inc, Waltham, MA) is the prototype of third-generation probes. Devised by Jeffcoat et al16 in 1986, this probe has controlled probing pressure and automated detection of the cementoenamel junction (CEJ). The components of the probe are: a pneumatic cylinder, a linear variable differential transducer (LVDT), a force transducer, an accelerator, and a probe tip.
The main mechanism of action of the Foster-Miller probe is by detection of the CEJ. The ball tip moves or glides over the root surface at a controlled speed and preset pressure. Abrupt changes in the acceleration of the probe movement (recorded on a graph) indicate when it meets the CEJ and when it is stopped at the base of the pocket. Under controlled pressure, the probe tip is extended into the pocket and refracted automatically when the base of the pocket is reached. Position and acceleration-time histories are analyzed to determine attachment level and pocket depth. As with all devices, the Foster-Miller probe has advantages and disadvantages. The main advantage is the automatic detection of the CEJ, which is a better landmark than gingival margin, because the position of the gingival margin may change depending on inflammation or recession.17 The main disadvantage is that it can deem root roughness or root surface irregularities as the CEJ.16
The Florida Probe® (Florida Probe Corp, www.floridaprobe.com) was devised by Gibbs et al18 in 1988. This probe consists of a probe handpiece and sleeve; a displacement transducer; a foot switch; and a computer interface/personal computer. The hemispheric probe tip has a diameter of 0.45 mm, and the sleeve has a diameter of 0.97 mm (Figure 3). Constant probing pressure of 15 gm is provided by coil springs inside the handpiece. The edge of the sleeve is the reference from which measurements are made, and the probe has Williams' markings; however, actual measurement of the pocket depth is made electronically and transferred automatically to the computer when the foot switch is pressed.
These probes provide a constant probing pressure of 15 gm, which can be overridden when necessary, for accuracy and patient comfort. They also can record missing teeth, recession, pocket depth, bleeding, suppuration, furcation involvement, mobility, and plaque assessment.19 Each measurement is recorded with potentially 0.2-mm accuracy. Comparison to previous data can be made more quickly and accurately. (The system shows black arrows for changes between 1 mm and 2 mm, and red arrows are used for changes > 2 mm.) Also, there is a chart showing diseased sites, which can be used in patient education.19 The Florida Probe does have some disadvantages, which include underestimating deep probing depths a lack of tactile sensitivity. Also, clinicians need to be trained to operate these probes.20
The Toronto Automated probe, devised by McCulloch and Birek in 1991 at University of Toronto, used the occlusoincisal surface to measure relative clinical attachment levels.21 The sulcus is probed with a 0.5-mm nickel-titanium wire that is extended under air pressure. It controls angular discrepancies by means of a mercury tilt sensor that limits angulation within ± 30º. This probe has the advantage of an incorporated electronic guidance system to improve precision in probe angulation. It also estimates the biophysical integrity of the dentogingival junction by measuring intrapocket probing velocity.22 The disadvantages are associated with positioning: It is difficult to measure second and third molars, and patients have to position their heads in the same place to reproduce readings.23
The InterProbe™ (The Dental Probe Inc, www.interprobe.com), also known as the Perio Probe, is a third-generation probe with a flexible probe tip, which curves with the tooth as the probes enter the pocket area.17 Stainless steel probes push the gingiva away from the tooth, causing pain, whereas the InterProbe gently slides in. The probe produces accurate readings of periodontal pockets with its standardized 15 gm of pressure. The probe's optical encoder handpieces uses constant probing pressure, which provides repeatable measurement of pocket depth and attachment loss.
Fourth-Generation Probes
Fourth-generation refers to three-dimensional (3D) probes. Currently under development, these probes are aimed at recording sequential probe positions along the gingival sulcus. They are an attempt to extend linear probing in a serial manner to take into account the continuous and 3D pocket being examined.7
Fifth-Generation Probes
Despite all the advances in earlier generation probes, they remain invasive and, at times, their use can be painful to patients. Plus, with these earlier generation probes, the probe tip usually crosses the junctional epithelium. Fifth-generation probes are being devised to eliminate these disadvantages. Probes are being designed to be 3D and noninvasive: an ultrasound or other device is added to a fourth-generation probe. Fifth-generation probes aim to identify the attachment level without penetrating it.
The only fifth-generation probe available, the UltraSonographic (US) probe (Visual Programs, Inc, www.usprobe.com), uses ultrasound waves to detect, image, and map the upper boundary of the periodontal ligament and its variation over time as an indicator of the presence of periodontal disease. The US probe was devised by Hinders and Companion at the NASA Langley Research Center.24 This small intraoral probe has an ultrasound beam projection area close enough in size to the width of the periodontal ligament space to give the optimal coupling and small enough to inspect the area between the teeth, while still delivering sufficient signal strength and depth of penetration to image the periodontal ligament space. To probe these structures ultrasonically, a narrow beam of ultrasonic energy is projected down between the tooth and bone from a transducer, which is scanned manually along the gingival margin. The transducer is mounted at the base of a dual-taper, convergent-divergent coupler to provide an acoustically tapered interface with a throat area on the order of 0.5 mm. This constitutes an active area reduction from the transducer element to the aperture of 20:1. Such a reduction is mandated by the geometry and the very small window afforded by the gingival margin. An added virtue of attaining this small a tip size is the ability of the ultrasonic probe to help the clinician examine the area between the teeth, which is where periodontal disease is most likely to occur.
The ultrasound transducer is mounted in the probe-tip shell, which also incorporates a slight flow of water to ensure good coupling of the ultrasonic energy to the tissues. The couplet water can come either from a suspended intravenous-type sterile bag or plumbed from the dental-unit water source. The focused ultrasonic beam is transmitted into the pocket in the same orientation as the insertion of a manual probe Then, the probe is moved along the gingival margin, so the two-dimensional graphical output corresponds to the results a clinician gets from "walking the sulcus" with a manual probe. However, ultrasound gives more information because secondary echoes are recorded from tissue features at various depths. It appears likely that the technique also will be able to provide information on the condition of the gingival tissue and the quality and extent of the epithelial attachment to the tooth surface. This may supply valuable data to aid the clinician in the diagnosis and treatment charting of these diseases.25
Nonperiodontal Probes
Calculus Detection
Calculus detection probes detect subgingival calculus by means of audio readings and are reported to increase chances of subgingival calculus detection.26 Currently, the DetecTar probe (DENTPLY Professional, www.dentsply.com) is the only calculus detection probe on the market. This device has a lightweight, well-balanced handpiece, which can be autoclaved, and it produces an audible beep to signify calculus detection (beep function can be disengaged). This probe may augment standard methods of calculus detection; however, it is expensive and the handpiece is bulkier than a standard periodontal probe. The probe has a short waterline hookup, which may prevent ergonomic placement of the unit, and it does not have a published waterline treatment protocol. As with many automated probes, there is potential for false positives and false negatives; therefore, further research is required.
Periodontal Disease Evaluation System
The Diamond Probe®/Perio 2000® System (Diamond General Development Corp, www.lifesciencesworld.com) reportedly detects periodontal disease during routine dental examinations by measuring relative sulfide concentrations as an indicator of gram-negative bacterial activity. The system consists of a single-use disposable probe tip with microsensors connected to a main control unit.27 The probe might detect periodontal disease at an early stage and might find an active site that requires treatment. However, the probing pressure is not controlled. Also, periodontal disease can be caused by bacteria that do not produce volatile sulfur compounds, creating the potential for some disease activity to be missed.28
The Periotemp® Probe (Abiodent Inc) is a temperature-sensitive probe, which reportedly detects early inflammatory changes in the gingival tissues by measuring temperature variations in these tissues.29 The Periotemp Probe detects pocket temperature differences of 0.1oC from a referenced subgingival temperature.30 This probe has two light indicating diodes: red-emitting diode, which indicates higher temperature, denoting risk is twice as likely for future attachment loss; and green-emitting diode, which indicates a lower temperature, indicating lower risk. This probe can detect initial inflammatory changes; therefore, treatment can be initiated at an early stage.30 However, the presence of surface cooling caused by breath airflow may further complicate the determination of even a normal temperature distribution.31
Conclusion
Newer developments in the field of periodontal probes provide the potential for error-free determination of pocket depth and clinical attachment level at a very early stage. Screening periodontal diseases earlier is gaining importance as these diseases are being associated with systemic conditions. With more research and innovation, the advent of newer error-free probes may resolve the remaining problems and those yet to be realized.
References
1. Orban B, Wentz FM, Everett FG, et al. Periodontics—A Concept: Theory and Practice. St Louis, MO: C.V. Mosby Co; 1958:103.
2. Wilkins EM. Examination procedures. In: Wilkins EM. Clinical Practice of the Dental Hygienist. 9th ed. Philadelphia, PA: Lippincott Williams and Wilkins; 2005:222-245.
3. Badersten A, Nilvéus R, Egelberg J. Reproducibility of probing attachment level measurements. J Clin Periodontol. 1984;11(7):475-485.
4. Listgarten MA, Mao R, Robinson PJ. Periodontal probing and the relationship of the probe tip to periodontal tissues. J Periodontol. 1976;47(9):511-513.
5. Parakkal PF. Proceedings of the workshop on quantitative evaluation of periodontal diseases by physical measurement techniques. J Dent Res. 1979;58(2):547-553.
6. Pihlstrom BL. Measurement of attachment level in clinical trials: Probing methods. J Periodontol. 1992;63(12 Suppl):1072-1077.
7. Watts TLP. Assessing periodontal health and disease. In: Periodontics in Practice: Science with Humanity. New York, NY: Informa Healthcare; 2000:33-40.
8. Williams CHM. Some newer periodontal findings of practical importance to the general practitioner. J Can Dent Assoc. 1936;2:333-340.
9. World Health Organization. Epidemiology, Etiology and Prevention of Periodontal Diseases. Report of a WHO Scientific Group. Geneva, Switzerland: World Health Organization; 1978. Technical Report Series No. 621.
10. Hefti AF. Periodontal probing. Crit Rev Oral Biol Med. 1997;8(3):336-356.
11. Birek P, McCulloch CAG, Hardy V. Gingival attachment level measurements with an automated periodontal probe. J Clin Periodontol. 1987;14(8):472-477.
12. Armitage GC, Svanberg GK, Löe H. Microscopic evaluation of clinical measurements of connective tissue attachment levels. J Clin Periodontol. 1977;4(3):173-190.
13. Van der Velden U, de Vries IH. Introduction of a new periodontal probe: the pressure probe. J Clin Periodontol. 1978;5(3):188-197.
14. Polson AM, Caton IB, Yeaple RN, et al. Histological determination of probe tip penetration into gingival sulcus of humans using an electronic pressure sensitive probe. J Clin Periodontol. 1980;7(6):479-488.
15. Kleinberg I, Kaufman HW, Wolff M. Measurement of tooth hypersensitivity and oral factors involved in its development. Arch Oral Biol. 1994;39(Suppl):63S-71S.
16. Jeffcoat MK, Jeffcoat RL, Jens SC, et al. A new periodontal probe with automated cemento-enamel junction detection. J Clin Periodontol. 1986;13(4):276-280.
17. Jeffcoat MK. Diagnosing periodontal disease: new tools to solve an old problem. J Am Dent Assoc. 1991;122(1):54-59.
18. Gibbs CH, Hirschfeld IW, Lee JG, et al. Description and clinical evaluation of a new computerized periodontal probe-the Florida Probe. J Clin Periodontol. 1988;15(2):137-144.
19. Osborn JB, Stoltenberg JL, Huso BA, et al. Comparison of measurement variability in subjects with moderate periodontitis using a conventional and constant force periodontal probe. J Periodontol. 1992;63(4):283-289.
20. Perry DA, Taggart EJ, Leung A, et al. Comparison of a conventional probe with electronic and manual pressure-regulated probes. J Periodontol. 1994;65(10):908-913.
21. McCulloch CA, Birek P. Automated probe: futuristic technology for diagnosis of periodontal disease. Univ Toronto Dent J. 1991;4(2):6-8.
22. Tessier JF, Kulkarni GV, Ellen RP, et al. Probing velocity: novel approach for assessment of inflamed periodontal attachment. J Periodontol. 1994;65(2):103-108.
23. Mariano S. Advanced diagnostic techniques. In: Newman MG, Takei H, Carranza FA, et al. Carranza's Clinical Periodontology.10th ed. Philadelphia, PA: Saunders; 2006:579-598.
24. Hinders M, Companion J. Ultrasonic probe for periodontal Disease. In: Thompson DO, Chimenti DE. Reviews of Progress in Quantitative Nondestructive Evaluation. Volume 18. New York, NY: Plenum Publishing; 1999:1609.
25. Hinders M, Hou J. Dynamic Wavelet fingerprint identification of ultrasound signals. Materials Evaluation. 2002;60(9):1089-1093.
26. Kasaj A, Moschos I, Röhrig B, et al. The effectiveness of a novel optical probe in subgingival calculus detection. Int J Dent Hyg. 2008;6(2):143-147.
27. Zhou H, McCombs GB, Darby ML, et al. Sulphur by-product: the relationship between volatile sulphur compounds and dental plaque-induced gingivitis. J Contemp Dent Pract. 2004;5(2):27-39.
28. McNamara TF, Alexander JF, Lee M. The role of microorganisms in the production of oral malodor. Oral Surg Oral Med Oral Pathol. 1972;34(1):41-48.
29. Kung RT, Ochs B, Goodson JM. Temperature as a periodontal diagnostic. J Clin Periodontol. 1990;17(8):557-563.
30. Haffajee AD, Socransky SS, Goodson JM. Subgingival temperature (I). relation to baseline clinical parameters. J Clin Periodontol. 1992;19(6):401-408.
31. Kung RTV, Goodson JM. Diagnostic temperature probe. Available at: https://www.freepatentsonline.com/result.html?query_txt=PN/EP0349581%20OR%20EP0349581AO. Accessed Oct 18, 2008.
About the Authors
Srinivas Sulugodu Ramachandra, MDS
Senior Lecturer, Department of Periodontology, Kanti Devi Dental College and Hospital
Mathura-Delhi,
Uttar Pradesh, India
Dhoom Singh Mehta, MDS
Professor and Head, Vice Principal, Department of Periodontology and Implantology, Bapuji Dental College and Hospital, Davangere,
Karnataka, India
Nagarajappa Sandesh MDS Senior Lecturer, Department of Community Dentistry, Kanti Devi Dental College and Hospital, Mathura-Delhi,
Uttar Pradesh, India
Vidya Baliga, MDS
Senior Lecturer, Department of Periodontology, Kanti Devi Dental College and Hospital, Mathura-Delhi, Uttar Pradesh, India
Janardhan Amarnath, MDS
Reader, Department of Periodontology, Kanti Devi Dental College and Hospital, Mathura-Delhi
Uttar Pradesh, India